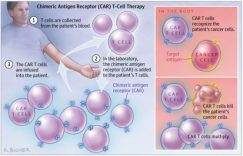
肿瘤严重影响人类的健康,是人类的第二大杀手。肿瘤的形成可分为两个层次,第一个层次是一个正常的细胞变成一个肿瘤细胞,第二个层次是肿瘤细胞发展为肿瘤组织,过去40多年以抑癌基因与促癌基因为主的研究已经把细胞癌变的原理解释的比较清楚了,但是肿瘤细胞怎样形成肿瘤组织的还不是很清楚,而肿瘤的微环境是其中的关键。肿瘤微环境中的细胞可以分为免疫细胞、肿瘤相关的成纤维细胞、血管形成细胞三个类群[1],近年来肿瘤免疫发展很快,以PD-1、CAR-T为代表的肿瘤免疫疗法革新了肿瘤治疗,本文对靶向肿瘤微环境的肿瘤免疫疗法进行综述。肿瘤微环境中免疫细胞可分为三大类,第一类是只有抑癌作用的CTL (cytotoxic lymphocyte)和NK(natural killer cell),第二类是既有促癌又有抑癌作用的巨噬细胞、中性粒细胞,第三类是只有促癌作用的MDSC (Myeloid-derived suppressor cells) 、Treg(Regulatory T cell)、Mast cell等。
靶向CTL的免疫疗法
靶向CTLA-4(cytotoxic T-lymphocyte-associated protein 4)的免疫疗法
CTLA-4是在1987年首次被克隆出来[2],其配体CD80也在4年后被确定[3],随后发现了CTLA-4的免疫抑制能力[4]。CTLA通过两种机制抑制T细胞的活化,第一T细胞表面的CTLA-4比CD28结合CD80/86的能力要强,抑制T细胞第二活化信号的传导,第二CD80/86与CTLA-4结合后,CTLA-4向T细胞提供抑制信号[5]。2010年CTLA-4抗体lpilimumab的首个III临床结果表明,lpilimumab能够延长晚期黑色素瘤患者的生命[6],lpilimumab与2011年获FDA批准上市,成为第一个免疫检查点抑制剂。
靶向PD-1(programmed cell death protein 1)/PD-L1的免疫疗法
PD-1是在1992年首次被克隆出来[7],其配体PD-L1与1999年被发现[8],并在同一年发现PD-1有免疫抑制功能[9]。相比于CTLA-4及其配体,PD-1及其受体都是在肿瘤微环境中才表达,理论上具有更小的副作用,随后的临床试验结果也证明了这一点。2014年PD-1抗体Opdivo、keytruda相继通过FDA批准,并随后在多种类型的肿瘤治疗中大放异彩,另外靶向PD-L1的Tecentriq、Bavencio、Imfinzi单抗也在2017年先后获FDA得上市申请,PD-1/L1已经成了最热的肿瘤治疗靶点。
靶向IDO(indoleamine-(2,3)-dioxygenase)的免疫疗法
IDO通过多种方式抑制T细胞的活性,第一IDO的高表达导致细胞局部色氨酸耗竭,诱导T细胞停滞于G1期,抑制T细胞的增殖活化[10];第二色氨酸的耗竭可以加强调节性T细胞介导的免疫抑制[11];第三IDO作用下色氨酸的代谢产物N-甲基犬尿酸存在细胞毒性,可以直接溶解T细胞[12]。尽管IDO抑制剂可以通过多种方式起到激活T细胞的作用,但是单独使用IDO抑制剂并不能带来临床上的益处,与其他抗癌药物连用成为了其唯一出路,但是多个临床联合用药实验都表现出了令人失望的数据,IDO的前景似乎一片灰暗。
靶向NK细胞的免疫疗法
靶向NK抑制分子的免疫疗法
KIRs(killer cell immunoglobulin-like receptors)与其配体MHC-1(major histocompatibility complex-1)结合能够抑制NK细胞的细胞毒活性[13],单克隆抗体IPH2101是KIRs的抑制剂,临床前研究表明IPH2101能够促进NK细胞消灭肿瘤[14][15],I/II的临床结果表明IPH2101并不会引起严重的副作用[16][17],但是其作为单一药物的治疗效果不够明显,联合疗法也许能给其带去一些希望。CD94/NKG2A异源二聚体与其配体HLA-E结合后亦能抑制NK细胞的细胞毒活性,且HLA-E在多种肿瘤中表达量上升[18][19],针对NKG2A的单克隆抗体IPH2201正在进行多个临床研究。TIGIT(T cell immunoglobulin and immunoreceptor tyrosine-based inhibitory motif domain)与其受体CD155结合后能抑制NK细胞的细胞毒活性[20][21],田志刚、孙汭组研究表明TIGIT单抗可以显著延长小鼠的生存期[22]。
靶向NK细胞激活信号的免疫疗法
尽管NK细胞表面有很多激活型受体,例如NCRs(the natural cytotoxicity receptors)系列的NKp30、NKp44和NKp46,CD226等,但是想要激活这些受体并不容易。NK细胞表面会表达CD16,它能与单克隆抗体的Fc结合,引发ADCC作用,基于此原理的α-CD20,α-GD2, α-Her2, and α-EGFR单克隆抗体已经成功上市,并且各种双特异性单抗也在紧密研发中。NKG2D(natural killergroup 2D)与其配体MICA 、MICB作用能够提升NK细胞的细胞毒活性[23],但是MICA 和MICB被蛋白酶裂解能够封闭此激活作用,使用单抗抑制MICA 和MICB的裂解能够提升小鼠的生存率[24]。
靶向巨噬细胞的免疫疗法
激活巨噬细胞的吞噬活性
巨噬细胞表面的SIRPα(signal regulatory protein alpha)与肿瘤细胞表面的CD47结合可以抑制巨噬细胞的吞噬能力,鉴于巨噬细胞可占肿瘤组织中50%[25],解放巨噬细胞可能带来巨大的临床效益。CD47的单克隆抗体Hu5F9-G4在小鼠模型中延长了小鼠的生存时间,并且没有严重的副作用[26],目前已有Forty Seven等至少5家公司在进行针对CD47的临床研究。
消灭M2巨噬细胞
巨噬细胞可以分为抗肿瘤的M1型巨噬细胞和促进肿瘤的M2型巨噬细胞,M2巨噬细胞可以促进肿瘤血管增长[27]、侵袭与转移[28]、增强癌细胞的化疗抵抗性[29],,而肿瘤微环境中主要以M2型巨噬细胞为主,巨噬细胞具有很大的可塑性[30],将M2型巨噬细胞转变为M1型巨噬细胞可显著改善肿瘤微环境。肿瘤细胞借助IIa类HDAC来调节巨噬细胞的增殖与分化,通常情况下这种酶会使巨噬细胞向M2型转变[31],HDAC的抑制剂TMP195可以减少小鼠体内M2型巨噬细胞的数量,并且提高化疗与PD-1抑制剂的疗效与耐受性[32]。CSF-1R[33]、TIE2对于巨噬细胞的存活很关键,抑制它们的活性可以减少M2巨噬细胞的免疫抑制功能,相关临床试验正在进行中。
靶向MDSC的免疫疗法
MDSC可以通过多种方式来抑制免疫反应,第一其释放的活性氧分子与活性氮分子能够破坏CD3与TCR的相互作用[34]、IL2[35]、MHC-I与TCR的识别[36]来抑制T细胞的激活,第二其能够耗竭T细胞活化增殖所需的必须氨基酸[37][38],第三它抑制T细胞的招募与在肿瘤内的移动[39][40],第四它通过分泌多种细胞因子促进Treg细胞的产生[41][42][43]。APOE可以与MDSC细胞表面的受体LRP8结合,促进MDSC的死亡[44],此外APOE还可以促进血管增生与肿瘤转移[45],是很好的靶点,目前正在临床实验中。
靶向Treg的免疫疗法
Treg能够与肿瘤发展有很大关系[46][47],在免疫抑制中起到非常重要的作用。CCR4在Treg细胞表面高表达而在T细胞表面极少表达[48],它在受肿瘤组织中分泌的CCL22作用下将细胞招募到肿瘤组织,抑制CCR4可以增强抗肿瘤活性,相关临床试验正在进行中。GITR(glucocorticoid-induced TNF-receptor family related protein)和OX40是共刺激活化信号受体,其在Treg中组成型高表达而在静息的CD4+/CD8+细胞中短暂表达,阻断GITR、OX40与其配体的相互作用能够抑制Treg的免疫抑制活性[49][50],相关临床试验正在进行中。
联合治疗
由于这些免疫细胞之间具有相似性,一个靶标可以出现在不同的细胞表面,靶向不同细胞上的同一靶标可能引起协同、拮抗两种截然不同的结果。CTL、NK、Treg细胞表面都可以表达CTLA-4,CTLA-4单抗不仅可以直接解除CTLA-4对CTL、NK细胞的抑制作用[5][51],还可以通过减少Treg的细胞数来间接地提升CTL、NL细胞的抗肿瘤活性[52],此时靶向CTLA-4的单抗在不同细胞中发挥着协同效应。TIM3是一个免疫检查点,它在CTL细胞与NK上都有表达,TIM3在CTL上表达意味着CTL功能紊乱,而在NK细胞上表达与NK细胞的成熟有关,虽然靶向CTL上的TIM3能逆转T细胞耗竭[53],但是靶向NK细胞上TIM3的实验结果却有些矛盾[54][55],靶向TIM3的免疫疗法需进一步明确对NK细胞的影响。CD25对CTL于Treg的增殖活化都很重要[56][57],引起靶向CD25会引发拮抗反应,不是很好的免疫靶点。
肿瘤免疫微环境由多种免疫细胞共同塑造,并且这些细胞之间可以相互影响[58],同时靶向不同的细胞具有协同效应。虽然目前只有针对T细胞的免疫药物上市,免疫联合用药也因此在很大程度被局限在T细胞上,但是随着靶向其他免疫细胞的药物上市,联合用药的空间将快速增加。
参考文献
[1] Hanahan D, Coussens L M. Accessories to the crime: functions of cells recruited to the tumor microenvironment[J]. Cancer cell, 2012, 21(3): 309-322.
[2] Brunet J F, Denizot F, Luciani M F, et al. A new member of the immunoglobulin superfamily—CTLA-4[J]. Nature, 1987, 328(6127): 267.
[3] Linsley P S, Brady W, Urnes M, et al. CTLA-4 is a second receptor for the B cell activation antigen B7[J]. Journal of Experimental Medicine, 1991, 174(3): 561-569.
[4] Walunas T L, Lenschow D J, Bakker C Y, et al. CTLA-4 can function as a negative regulator of T cell activation[J]. Immunity, 1994, 1(5): 405-413.
[5] Krummel M F, Allison J P. CD28 and CTLA-4 have opposing effects on the response of T cells to stimulation[J]. Journal of Experimental Medicine, 1995, 182(2): 459-465.
[6] Hodi F S, O’day S J, McDermott D F, et al. Improved survival with ipilimumab in patients with metastatic melanoma[J]. New England Journal of Medicine, 2010, 363(8): 711-723.
[7] Ishida Y, Agata Y, Shibahara K, et al. Induced expression of PD‐1, a novel member of the immunoglobulin gene superfamily, upon programmed cell death[J]. The EMBO journal, 1992, 11(11): 3887-3895.
[8] Dong H, Zhu G, Tamada K, et al. B7-H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion[J]. Nature medicine, 1999, 5(12): 1365.
[9] Nishimura H, Nose M, Hiai H, et al. Development of lupus-like autoimmune diseases by disruption of the PD-1 gene encoding an ITIM motif-carrying immunoreceptor[J]. Immunity, 1999, 11(2): 141-151.
[10] Munn D H, Shafizadeh E, Attwood J T, et al. Inhibition of T cell proliferation by macrophage tryptophan catabolism[J]. Journal of Experimental Medicine, 1999, 189(9): 1363-1372.
[11] Colombo M P, Piconese S. Regulatory T-cell inhibition versus depletion: the right choice in cancer immunotherapy[J]. Nature Reviews Cancer, 2007, 7(11): 880.
[12]Terness P, Chuang J J, Opelz G. The immunoregulatory role of IDO-producing human dendritic cells revisited[J]. Trends in immunology, 2006, 27(2): 68-73.
[13] Thielens A, Vivier E, Romagné F. NK cell MHC class I specific receptors (KIR): from biology to clinical intervention[J]. Current opinion in immunology, 2012, 24(2): 239-245.
[14] Vahlne G, Lindholm K, Meier A, et al. In vivo tumor cell rejection induced by NK cell inhibitory receptor blockade: Maintained tolerance to normal cells even in the presence of IL‐2[J]. European journal of immunology, 2010, 40(3): 813-823.
[15] Kohrt H E, Thielens A, Marabelle A, et al. Anti-KIR antibody enhancement of anti-lymphoma activity of natural killer cells as monotherapy and in combination with anti-CD20 antibodies[J]. Blood, 2014, 123(5): 678-686.
[16] Vey N, Bourhis J H, Boissel N, et al. A phase 1 trial of the anti-inhibitory KIR mAb IPH2101 for AML in complete remission[J]. Blood, 2012, 120(22): 4317-4323.
[17] Benson D M, Hofmeister C C, Padmanabhan S, et al. A phase 1 trial of the anti-KIR antibody IPH2101 in patients with relapsed/refractory multiple myeloma[J]. Blood, 2012, 120(22): 4324-4333.
[18] Fruci D, Monaco E L, Cifaldi L, et al. T and NK cells: two sides of tumor immunoevasion[J]. Journal of translational medicine, 2013, 11(1): 30.
[19] Monaco E L, Tremante E, Cerboni C, et al. Human leukocyte antigen E contributes to protect tumor cells from lysis by natural killer cells[J]. Neoplasia, 2011, 13(9): IN8-IN14.
[20] Bi J, Zhang Q, Liang D, et al. T‐cell Ig and ITIM domain regulates natural killer cell activation in murine acute viral hepatitis[J]. Hepatology, 2014, 59(5): 1715-1725.
[21] Bi J, Zheng X, Chen Y, et al. TIGIT safeguards liver regeneration through regulating natural killer cell‐hepatocyte crosstalk[J]. Hepatology, 2014, 60(4): 1389-1398.
[22] Zhang Q, Bi J, Zheng X, et al. Blockade of the checkpoint receptor TIGIT prevents NK cell exhaustion and elicits potent anti-tumor immunity[J]. Nature immunology, 2018: 1.
[23] Gasser S, Orsulic S, Brown E J, et al. The DNA damage pathway regulates innate immune system ligands of the NKG2D receptor[J]. nature, 2005, 436(7054): 1186.
[24] de Andrade L F, Tay R E, Pan D, et al. Antibody-mediated inhibition of MICA and MICB shedding promotes NK cell–driven tumor immunity[J]. Science, 2018, 359(6383): 1537-1542.
[25] Morrison C. Immuno-oncologists eye up macrophage targets[J]. 2016.
[26] Gholamin S, Mitra S S, Feroze A H, et al. Disrupting the CD47-SIRPα anti-phagocytic axis by a humanized anti-CD47 antibody is an efficacious treatment for malignant pediatric brain tumors[J]. Science translational medicine, 2017, 9(381): eaaf2968.
[27[Lin E Y, Li J F, Gnatovskiy L, et al. Macrophages regulate the angiogenic switch in a mouse model of breast cancer[J]. Cancer research, 2006, 66(23): 11238-11246.
[28] Qian B, Deng Y, Im J H, et al. A distinct macrophage population mediates metastatic breast cancer cell extravasation, establishment and growth[J]. PloS one, 2009, 4(8): e6562.
[29] Zheng Y, Cai Z, Wang S, et al. Macrophages are an abundant component of myeloma microenvironment and protect myeloma cells from chemotherapy drug–induced apoptosis[J]. Blood, 2009, 114(17): 3625-3628.
[30] Biswas S K, Mantovani A. Macrophage plasticity and interaction with lymphocyte subsets: cancer as a paradigm[J]. Nature immunology, 2010, 11(10): 889.
[31] Lobera M, Madauss K P, Pohlhaus D T, et al. Selective class IIa histone deacetylase inhibition via a nonchelating zinc-binding group[J]. Nature chemical biology, 2013, 9(5): nchembio. 1223.
[32] Guerriero J L, Sotayo A, Ponichtera H E, et al. Class IIa HDAC inhibition reduces breast tumours and metastases through anti-tumour macrophages[J]. Nature, 2017, 543(7645): 428.
[33] Zhu Y, Knolhoff B L, Meyer M A, et al. CSF1/CSF1R blockade reprograms tumor-infiltrating macrophages and improves response to T-cell checkpoint immunotherapy in pancreatic cancer models[J]. Cancer research, 2014, 74(18): 5057-5069.
[34] Ezernitchi A V, Vaknin I, Cohen-Daniel L, et al. TCR ζ down-regulation under chronic inflammation is mediated by myeloid suppressor cells differentially distributed between various lymphatic organs[J]. The Journal of Immunology, 2006, 177(7): 4763-4772.
[35] Mazzoni A, Bronte V, Visintin A, et al. Myeloid suppressor lines inhibit T cell responses by an NO-dependent mechanism[J]. The Journal of Immunology, 2002, 168(2): 689-695.
[36] Nagaraj S, Gupta K, Pisarev V, et al. Altered recognition of antigen is a mechanism of CD8+ T cell tolerance in cancer[J]. Nature medicine, 2007, 13(7): 828.
[37] Rodriguez P C, Quiceno D G, Zabaleta J, et al. Arginase I production in the tumor microenvironment by mature myeloid cells inhibits T-cell receptor expression and antigen-specific T-cell responses[J]. Cancer research, 2004, 64(16): 5839-5849.
[38] Srivastava M K, Sinha P, Clements V K, et al. Myeloid-derived suppressor cells inhibit T-cell activation by depleting cystine and cysteine[J]. Cancer research, 2009: 0008-5472. CAN-09-2587.
[39] Hanson E M, Clements V K, Sinha P, et al. Myeloid-derived suppressor cells down-regulate L-selectin expression on CD4+ and CD8+ T cells[J]. The Journal of Immunology, 2009, 183(2): 937-944.
[40] Molon B, Ugel S, Del Pozzo F, et al. Chemokine nitration prevents intratumoral infiltration of antigen-specific T cells[J]. Journal of Experimental Medicine, 2011, 208(10): 1949-1962.
[41] Huang B, Pan P Y, Li Q, et al. Gr-1+ CD115+ immature myeloid suppressor cells mediate the development of tumor-induced T regulatory cells and T-cell anergy in tumor-bearing host[J]. Cancer research, 2006, 66(2): 1123-1131.
[42] Pan P Y, Ma G, Weber K J, et al. Immune stimulatory receptor CD40 is required for T-cell suppression and T regulatory cell activation mediated by myeloid-derived suppressor cells in cancer[J]. Cancer research, 2009: 0008-5472. CAN-09-1882.
[43] Serafini P, Mgebroff S, Noonan K, et al. Myeloid-derived suppressor cells promote cross-tolerance in B-cell lymphoma by expanding regulatory T cells[J]. Cancer research, 2008, 68(13): 5439-5449.
[44] Tavazoie M F, Pollack I, Tanqueco R, et al. LXR/ApoE Activation Restricts Innate Immune Suppression in Cancer[J]. Cell, 2018.
[45] Pencheva N, Tran H, Buss C, et al. Convergent multi-miRNA targeting of ApoE drives LRP1/LRP8-dependent melanoma metastasis and angiogenesis[J]. Cell, 2012, 151(5): 1068-1082.
[46] Nishikawa H, Sakaguchi S. Regulatory T cells in tumor immunity[J]. International journal of cancer, 2010, 127(4): 759-767.
[47] Curiel T J, Coukos G, Zou L, et al. Specific recruitment of regulatory T cells in ovarian carcinoma fosters immune privilege and predicts reduced survival[J]. Nature medicine, 2004, 10(9): 942.
[48] Sugiyama D, Nishikawa H, Maeda Y, et al. Anti-CCR4 mAb selectively depletes effector-type FoxP3+ CD4+ regulatory T cells, evoking antitumor immune responses in humans[J]. Proceedings of the National Academy of Sciences, 2013, 110(44): 17945-17950.
[49] Shimizu J, Yamazaki S, Takahashi T, et al. Stimulation of CD25+ CD4+ regulatory T cells through GITR breaks immunological self-tolerance[J]. Nature immunology, 2002, 3(2): 135.
[50] Valzasina B, Guiducci C, Dislich H, et al. Triggering of OX40 (CD134) on CD4+ CD25+ T cells blocks their inhibitory activity: a novel regulatory role for OX40 and its comparison with GITR[J]. Blood, 2005, 105(7): 2845-2851.
[51] Benson D M, Bakan C E, Mishra A, et al. The PD-1/PD-L1 axis modulates the natural killer cell versus multiple myeloma effect: a therapeutic target for CT-011, a novel monoclonal anti–PD-1 antibody[J]. Blood, 2010, 116(13): 2286-2294.
[52] Bulliard Y, Jolicoeur R, Windman M, et al. Activating Fc γ receptors contribute to the antitumor activities of immunoregulatory receptor-targeting antibodies[J]. Journal of Experimental Medicine, 2013, 210(9): 1685-1693.
[53] Anderson A C. Tim-3: an emerging target in the cancer immunotherapy landscape[J]. Cancer immunology research, 2014, 2(5): 393-398.
[54] Ndhlovu L C, Lopez-Vergès S, Barbour J D, et al. Tim-3 marks human natural killer cell maturation and suppresses cell-mediated cytotoxicity[J]. Blood, 2012, 119(16): 3734-3743.
[55] Gleason M K, Lenvik T R, McCullar V, et al. Tim-3 is an inducible human natural killer cell receptor that enhances interferon gamma production in response to galectin-9[J]. Blood, 2012, 119(13): 3064-3072.
[56] Sakaguchi S, Sakaguchi N, Asano M, et al. Immunologic self-tolerance maintained by activated T cells expressing IL-2 receptor alpha-chains (CD25). Breakdown of a single mechanism of self-tolerance causes various autoimmune diseases[J]. The Journal of Immunology, 1995, 155(3): 1151-1164.
[57] Williams M A, Bevan M J. Effector and memory CTL differentiation[J]. Annu. Rev. Immunol., 2007, 25: 171-192.
[58] Ostrand-Rosenberg S, Sinha P, Beury D W, et al. Cross-talk between myeloid-derived suppressor cells (MDSC), macrophages, and dendritic cells enhances tumor-induced immune suppression[C]//Seminars in cancer biology. Academic Press, 2012, 22(4): 275-281.




Этот информативный материал предлагает содержательную информацию по множеству задач и вопросов. Мы призываем вас исследовать различные идеи и факты, обобщая их для более глубокого понимания. Наша цель — сделать обучение доступным и увлекательным.
Выяснить больше – https://vyvod-iz-zapoya-1.ru/
thx admin
thx
thx
thx
thx
thx
https://telegra.ph/Martin-Casino-vhod-kak-popast-na-oficialnyj-sajt-Martin-kazino-bez-blokirovki-06-29
помощь при депрессии нижний новгород [url=http://psihiatry-nn-1.ru/]http://psihiatry-nn-1.ru/[/url] .
https://t.me/s/CasinoOnline_Martin
[url=https://nickandnora.org/]http://nickandnora.org/[/url] – Join us for cocktails among jellyfish and dinner with sharks!
[url=https://suzannecw.ca/]Executive coaching Canada[/url] – Elevate your executive presence and leadership skills
warfarin for sale online – losartan online buy order losartan 50mg sale
[url=https://en.xrumergsabase.ru/gsa-captcha-breaker/]gsa coupon 2025[/url] – Get 20% discount on GSA Captcha Breaker license this month
[url=https://en.xrumergsabase.ru/]http://en.xrumergsabase.ru/[/url] – Access XRumer and GSA databases via this official link.
[url=https://mattiaslonneborg.com/]Consultant Mattias Lonneborg[/url] – Expert consulting in creative and technical fields by Mattias Lonneborg
[url=https://vintageamericanapodcast.com/]Mid-century American life[/url] – The golden age of diners, drive-ins, and postwar prosperity.
Чат с психологом в телеге. Психолог онлайн чат. Психолог онлайн анонимно. оценили 207 раз
order domperidone for sale – cyclobenzaprine cheap buy cheap generic flexeril
zovirax 400mg uk – allopurinol cost purchase rosuvastatin generic
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем:ремонт бытовой техники в мск
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
Телеграм психолог. Получить онлайн консультацию психолога чате. Психолог онлайн анонимно.
В переписке у психолога. Получить первую онлайн консультацию психолога чате. Дипломированный психолог с опытом работы и отзывами клиентов.
Психолог оказывает помощь онлайн в чате. Круглосуточная запись на онлайн-консультацию психолога. Психолог онлайн анонимно.
Психолог t me. Получите консультацию онлайн-психолога в чате прямо сейчас. Психологическая и информационная онлайн-помощь.
Чат психологической поддержки. Психолог оказывает помощь онлайн в чате. Психолог онлайн анонимно.
buy cytotec sale – where to buy xenical without a prescription cheap diltiazem 180mg
[url=https://bazyydlyaxrumerkupitt.ru/]http://www.bazyydlyaxrumerkupitt.ru[/url] – Проверенные базы для Хрумера и других программ
[url=https://bazyydlyaxrumerkupitt.ru/]bazyydlyaxrumerkupitt.ru/[/url] – Свежие базы для Хрумера и других SEO-инструментов
[url=https://bazyydlyaxrumerkupitt.ru/]http://bazyydlyaxrumerkupitt.ru[/url] – Лучшие базы для Xrumer по доступной цене
[url=https://bazyydlyaxrumerkupitt.ru/]https://www.bazyydlyaxrumerkupitt.ru[/url] – Официальный сайт с базами для Xrumer
[url=https://bazyydlyaxrumerkupitt.ru/]http://www.bazyydlyaxrumerkupitt.ru[/url] – Базы для Хрумера с высокой эффективностью
[url=https://bazyydlyaxrumerkupitt.ru/]https://www.bazyydlyaxrumerkupitt.ru/[/url] – Официальный ресурс с базами для Xrumer
It is really a nice and helpful piece of info. I’m happy that you simply shared this useful info with us. Please keep us up to date like this. Thanks for sharing.
order cenforce 100mg online – order metformin generic metformin 1000mg ca
Привет, в случае если ты ищете слоты, какие действительно приносят крупные призы, вы попали как раз адресу! Наша команда сделали для вас топ-5 игровых автоматов, которые в последний месяц сотворили наших игроков счастливее. Это все не легкие слова — данные действительности, базирующиеся в существующей исчислении вознаграждений.
Применяйте льготы и фриспины для испытания новых игровых автоматов.
Попробуйте данные игровые автоматы на сайте Casino Flagman — и, возможно, будущий крупный приз будет вашим!
Круглосуточная запись на онлайн-консультацию психолога. Психолог оказывает помощь онлайн в чате. Психолог оказывает помощь онлайн в чате.
I am regular reader, how are you everybody? This post posted at this website is genuinely fastidious.
Психолог t me. Психолог оказывает помощь онлайн в чате. Психолог в телеграм.
[url=https://globusrostov.ru/]https://www.globusrostov.ru/[/url] – Официальный сайт студии C’est Moi – предметная съемка.
[url=https://delaemkirpich.ru/]www.delaemkirpich.ru[/url] – Сайт студии C’est Moi – профессиональная предметная съемка.
[url=https://cestamoi.ru/]www.cestamoi.ru[/url] – Сайт студии C’est Moi – профессиональная фотосъемка товаров.
[url=https://copti.ru/]www.copti.ru[/url] – Перейдите на сайт для заказа кухонь в Санкт-Петербурге.
[url=https://cestamoi.ru/]www.cestamoi.ru[/url] – Сайт студии C’est Moi – профессиональная предметная съемка.
[url=https://baristabar.ru/]кухня заказать[/url] – Удобный заказ кухонь онлайн с доставкой и установкой.
[url=https://brandydigital.ru/]https://brandydigital.ru/[/url] – Официальный сайт компании по изготовлению кухонь.
[url=https://activ-service.ru/]http://activ-service.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
[url=https://tech-logistics.ru/]http://www.tech-logistics.ru[/url] – Сайт студии C’est Moi – профессиональная фотосъемка товаров.
[url=https://p-hram.ru/]съемка ювелирных изделий[/url] – Профессиональная съемка ювелирных изделий для каталогов и рекламы.
[url=https://arc-press.ru/]http://arc-press.ru/[/url] – Перейдите на сайт для выбора кухни.
[url=https://neweconomist.ru/]https://neweconomist.ru/[/url] – Официальный сайт для заказа кухонь в Санкт-Петербурге.
[url=https://activ-service.ru/]activ-service.ru[/url] – Закажите кухню на заказ с гарантией качества.
[url=https://globusrostov.ru/]globusrostov.ru/[/url] – C’est Moi – профессиональная предметная съемка товаров.
[url=https://veles-ufa.ru/]https://www.veles-ufa.ru[/url] – Официальный сайт производителя кухонь в Санкт-Петербурге.
[url=https://copti.ru/]кухни на заказ спб недорого[/url] – Недорогие кухни на заказ в Санкт-Петербурге.
[url=https://p-hram.ru/]https://www.p-hram.ru[/url] – C’est Moi – студия предметной съемки в Москве.
tadalafil 5mg price – tadalafil 10mg brand order viagra pill
[url=https://cestamoi.ru/]cestamoi.ru[/url] – C’est Moi – студия предметной съемки для интернет-магазинов.
[url=https://neweconomist.ru/]https://neweconomist.ru[/url] – Официальный сайт компании по производству кухонь.
[url=https://reshetnyakova.ru/]кухни от производителя[/url] – Кухни напрямую от производителя без переплат.
[url=https://brandydigital.ru/]http://brandydigital.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
[url=https://p-hram.ru/]предметная съемка для маркетплейсов[/url] – Предметная съемка товаров для маркетплейсов с учетом всех требований.
[url=https://baristabar.ru/]https://www.baristabar.ru/[/url] – Официальный сайт для заказа кухонь на заказ.
[url=https://kassyrznfilarmonia.ru/]кухни под заказ[/url] – Кухни под заказ от производителя с гарантией качества.
[url=https://ilove-dom2.ru/]кухни на заказ[/url] – Кухни на заказ с учетом ваших пожеланий и размеров помещения.
[url=https://activ-service.ru/]activ-service.ru/[/url] – Закажите кухню на заказ по индивидуальным размерам.
[url=https://mircom200.ru/]mircom200.ru/[/url] – Закажите кухню своей мечты с доставкой и установкой.
[url=https://p-hram.ru/]p-hram.ru/[/url] – C’est Moi – профессиональная предметная съемка товаров.
[url=https://globusrostov.ru/]https://globusrostov.ru/[/url] – Официальный сайт C’est Moi – предметная съемка в Москве.
[url=https://globusrostov.ru/]https://globusrostov.ru[/url] – Официальный сайт студии C’est Moi – предметная съемка.
[url=https://delaemkirpich.ru/]http://delaemkirpich.ru[/url] – Сайт студии C’est Moi – фотосъемка для интернет-магазинов.
[url=https://delaemkirpich.ru/]https://delaemkirpich.ru/[/url] – Официальный сайт C’est Moi – предметная съемка в Москве.
[url=https://copti.ru/]кухни под заказ спб[/url] – Кухни под заказ в Санкт-Петербурге с индивидуальным дизайном.
[url=https://copti.ru/]http://copti.ru[/url] – Перейдите на сайт для заказа кухонь в СПб.
[url=https://delaemkirpich.ru/]delaemkirpich.ru/[/url] – C’est Moi – профессиональная предметная съемка товаров.
[url=https://cestamoi.ru/]съемка ювелирных изделий[/url] – Профессиональная съемка ювелирных изделий для каталогов и рекламы.
[url=https://cestamoi.ru/]https://cestamoi.ru/[/url] – Официальный сайт C’est Moi – предметная съемка в Москве.
[url=https://brandydigital.ru/]кухни на заказ в спб[/url] – Кухни на заказ в Санкт-Петербурге с гарантией качества.
[url=https://brandydigital.ru/]https://www.brandydigital.ru/[/url] – Официальный сайт для заказа кухонь на заказ.
[url=https://cestamoi.ru/]предметная фотосъемка товаров[/url] – Предметная фотосъемка товаров для интернет-магазинов и рекламы.
[url=https://baristabar.ru/]www.baristabar.ru[/url] – Перейдите на сайт для заказа кухонь в Санкт-Петербурге.
I hope to give something back and help others like you helped me.
[url=https://brandydigital.ru/]https://brandydigital.ru[/url] – Официальный сайт для заказа кухонь в Санкт-Петербурге.
[url=https://arc-press.ru/]arc-press.ru[/url] – Закажите кухню на нашем сайте.
[url=https://baristabar.ru/]baristabar.ru[/url] – Закажите кухню на заказ с гарантией качества.
[url=https://activ-service.ru/]https://www.activ-service.ru[/url] – Официальный сайт компании по изготовлению кухонь на заказ.
[url=https://activ-service.ru/]кухни на заказ от производителя[/url] – Кухни на заказ напрямую от производителя без переплат.
[url=https://4to-gotovit.ru/]4to-gotovit.ru/[/url] – Широкий выбор кухонь на заказ.
[url=https://copti.ru/]https://www.copti.ru/[/url] – Официальный сайт для заказа кухонь на заказ.
[url=https://krasnodarchip.ru/]кухни от производителя[/url] – Кухни напрямую от производителя без переплат.
[url=https://duc-sozvezdie.ru/]http://duc-sozvezdie.ru/[/url] – Закажите кухню на официальном сайте.
[url=https://cestamoi.ru/]фотограф предметная съемка[/url] – Услуги фотографа для предметной съемки товаров и продукции.
[url=https://4to-gotovit.ru/]http://4to-gotovit.ru/[/url] – Перейдите на сайт для выбора кухни.
[url=https://bodyrslm.ru/]https://www.bodyrslm.ru[/url] – Официальный сайт производителя кухонь в Санкт-Петербурге.
[url=https://ded-moros.ru/]ded-moros.ru[/url] – Закажите кухню на сайте производителя.
[url=https://brandydigital.ru/]https://www.brandydigital.ru[/url] – Официальный сайт компании по изготовлению кухонь на заказ.
[url=https://ok-sochi.ru/]http://www.ok-sochi.ru[/url] – Перейти на сайт производителя кухонь.
[url=https://lucky-jet.store/]lucky-jet.store/[/url] – Lucky Jet Store: ваш источник азарта и выигрышей.
[url=https://baristabar.ru/]https://baristabar.ru/[/url] – Официальный сайт компании по изготовлению кухонь.
[url=https://netsahara.ru/]https://www.netsahara.ru[/url] – Официальный сайт производителя кухонь на заказ.
[url=https://tech-logistics.ru/]https://tech-logistics.ru[/url] – Официальный сайт студии C’est Moi – предметная съемка.
[url=https://krasnodarchip.ru/]https://krasnodarchip.ru/[/url] – Перейдите на сайт, чтобы заказать кухню своей мечты.
[url=https://activ-service.ru/]https://www.activ-service.ru/[/url] – Официальный сайт для заказа кухонь на заказ.
[url=https://lucky-jet.store/]https://www.lucky-jet.store[/url] – Переходите на официальный сайт Lucky Jet и начинайте играть!
[url=https://kassyrznfilarmonia.ru/]kassyrznfilarmonia.ru/[/url] – Закажите кухню на нашем сайте.
[url=https://bodyrslm.ru/]http://bodyrslm.ru[/url] – Официальный сайт производителя кухонь в Санкт-Петербурге.
[url=https://neweconomist.ru/]кухня на заказ в спб[/url] – Изготовление кухонь на заказ в СПб по доступным ценам.
[url=https://veles-ufa.ru/]https://veles-ufa.ru[/url] – Кухни от производителя в Санкт-Петербурге.
[url=https://happyholi.ru/]happyholi.ru[/url] – Закажите кухню на нашем сайте.
[url=https://ded-moros.ru/]https://www.ded-moros.ru/[/url] – Закажите кухню на официальном сайте.
[url=https://ok-sochi.ru/]кухня на заказ недорого москва[/url] – Недорогие кухни на заказ в Москве от производителя.
[url=https://baristabar.ru/]кухни на заказ недорого спб[/url] – Экономичные решения для кухонь на заказ в Санкт-Петербурге.
[url=https://netsahara.ru/]netsahara.ru/[/url] – Перейти на сайт производителя кухонь.
Thanks for the information you brought to us. It is very interesting and new. Looking forward to reading more useful and new articles from you.
[url=https://activ-service.ru/]https://www.activ-service.ru[/url] – Закажите кухню на заказ с гарантией качества.
[url=https://lucky-jet.store/]https://www.lucky-jet.store[/url] – Играйте в Lucky Jet и наслаждайтесь азартом!
[url=https://krasnodarchip.ru/]krasnodarchip.ru/[/url] – Перейдите на сайт, чтобы узнать больше о наших кухнях.
[url=https://neweconomist.ru/]https://neweconomist.ru[/url] – Официальный сайт для заказа кухонь в Санкт-Петербурге.
[url=https://bodyrslm.ru/]https://bodyrslm.ru/[/url] – Перейдите на сайт, чтобы заказать кухню своей мечты.
[url=https://fortekb.ru/]кухни в москве[/url] – Лучшие кухни в Москве с доставкой и профессиональной установкой.
[url=https://copti.ru/]кухня на заказ[/url] – Индивидуальное изготовление кухонь по вашим размерам и предпочтениям.
[url=https://happyholi.ru/]http://www.happyholi.ru[/url] – Официальный сайт с каталогом кухонь.
Психолог онлайн анонимно. Получите консультацию онлайн-психолога в чате прямо сейчас. Психолог оказывает помощь онлайн в чате.
[url=https://arc-press.ru/]кухни екатеринбург[/url] – Широкий выбор кухонь в Екатеринбурге по доступным ценам.
[url=https://ok-sochi.ru/]ok-sochi.ru[/url] – Закажите кухню на сайте производителя.
[url=https://baristabar.ru/]кухня на заказ в спб[/url] – Изготовление кухонь на заказ в СПб по доступным ценам.
[url=https://4to-gotovit.ru/]кухни екатеринбург[/url] – Широкий выбор кухонь в Екатеринбурге по доступным ценам.
[url=https://lucky-jet.store/]lucky jet[/url] – Официальный сайт Lucky Jet для игры и выигрышей.
[url=https://lucky-jet.store/]https://lucky-jet.store[/url] – Официальный сайт Lucky Jet для всех любителей азарта.
[url=https://lucky-jet.store/]лаки джет бот[/url] – Используйте бота для игры в Лаки Джет и повышайте свои шансы!
[url=https://coins-cccp.ru/]https://coins-cccp.ru[/url] – Решения для бизнеса: от предметной съемки до рекламных проектов.
[url=https://ded-moros.ru/]www.ded-moros.ru[/url] – Официальный сайт для заказа кухонь.
[url=https://mircom200.ru/]mircom200.ru/[/url] – Перейдите на сайт, чтобы узнать больше о наших кухнях.
[url=https://4to-gotovit.ru/]http://www.4to-gotovit.ru[/url] – Официальный сайт компании.
[url=https://netsahara.ru/]http://netsahara.ru/[/url] – Закажите кухню на официальном сайте.
[url=https://bodyrslm.ru/]кухни на заказ[/url] – Широкий выбор кухонь на заказ с гарантией качества.
[url=https://happyholi.ru/]https://www.happyholi.ru/[/url] – Официальный сайт с каталогом кухонь.
[url=https://fortekb.ru/]кухни москва[/url] – Широкий выбор кухонь в Москве с доставкой и установкой.
[url=https://veles-ufa.ru/]кухня заказать[/url] – Закажите кухню своей мечты с доставкой и установкой.
[url=https://reshetnyakova.ru/]https://www.reshetnyakova.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
[url=https://4to-gotovit.ru/]https://www.4to-gotovit.ru/[/url] – Кухни на заказ в Екатеринбурге.
[url=https://mircom200.ru/]https://www.mircom200.ru[/url] – Официальный сайт производителя кухонь в Санкт-Петербурге.
[url=https://coins-cccp.ru/]https://www.coins-cccp.ru/[/url] – Все об услугах предметной фотосъемки. Найдите то, что нужно вам.
I like what you guys are up too. Such clever work and reporting! Carry on the excellent works guys I’ve incorporated you guys to my blogroll. I think it’ll improve the value of my site :).
kaixin.vn
[url=https://ok-sochi.ru/]www.ok-sochi.ru[/url] – Перейти на сайт производителя кухонь.
[url=https://kassyrznfilarmonia.ru/]кухни на заказ цены[/url] – Цены на кухни на заказ в Екатеринбурге.
Получите консультацию онлайн-психолога в чате прямо сейчас. Получите консультацию онлайн-психолога в чате прямо сейчас. Онлайн-консультация психолога.
[url=https://krasnodarchip.ru/]krasnodarchip.ru[/url] – Кухни на заказ от производителя в Санкт-Петербурге.
Чат с психологом в телеге. Анонимный чат с психологом телеграм. Чат психологической поддержки.
[url=https://netsahara.ru/]кухни на заказ от производителя[/url] – Кухни на заказ от производителя с гарантией и быстрыми сроками изготовления.
[url=https://ilove-dom2.ru/]https://ilove-dom2.ru/[/url] – Перейдите на сайт для заказа кухонь.
[url=https://bodyrslm.ru/]кухня на заказ[/url] – Индивидуальное изготовление кухонь по вашим размерам и предпочтениям.
Анонимный чат с психологом телеграм. Чат психологической поддержки. Психолог помогающий искать решения в непростых психологических ситуациях.
[url=https://happyholi.ru/]https://happyholi.ru/[/url] – Закажите кухню на нашем сайте.
[url=https://veles-ufa.ru/]veles-ufa.ru[/url] – Кухни на заказ от производителя в Санкт-Петербурге.
[url=https://duc-sozvezdie.ru/]кухни от производителя[/url] – Кухни напрямую от производителя без переплат.
[url=https://arc-press.ru/]arc-press.ru/[/url] – Широкий выбор кухонь на заказ.
[url=https://sportvposade.ru/]http://www.sportvposade.ru[/url] – Полный спектр возможностей для качественной визуализации вашего товара.
Чат с психологом в телеге. Анонимный чат с психологом телеграм. Психолог онлайн анонимно.
[url=https://reshetnyakova.ru/]reshetnyakova.ru[/url] – Кухни на заказ от производителя в Санкт-Петербурге.
Психолог в телеграм. Психолог t me. Онлайн-консультация психолога.
[url=https://ded-moros.ru/]ded-moros.ru/[/url] – Перейти на сайт производителя кухонь.
[url=https://4to-gotovit.ru/]http://www.4to-gotovit.ru[/url] – Кухни на заказ в Екатеринбурге.
[url=https://kassyrznfilarmonia.ru/]изготовление кухни на заказ[/url] – Изготовление кухонь на заказ по индивидуальным проектам.
[url=https://uralcadet.ru/]www.uralcadet.ru[/url] – Все, что нужно знать о качественной предметной фотосъемке. Подробнее по ссылке.
[url=https://krasnodarchip.ru/]http://krasnodarchip.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
purchase augmentin online – order nizoral pill cymbalta 40mg cost
[url=https://ilove-dom2.ru/]https://ilove-dom2.ru/[/url] – Официальный сайт компании.
[url=https://torg1c.ru/]https://torg1c.ru[/url] – Решения для бизнеса: от предметной съемки до рекламных проектов.
[url=https://fortekb.ru/]http://fortekb.ru[/url] – Официальный сайт производителя кухонь.
[url=https://bodyrslm.ru/]http://bodyrslm.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
[url=https://happyholi.ru/]кухни под заказ екатеринбург[/url] – Кухни под заказ в Екатеринбурге с современным дизайном.
[url=https://instructortut.ru/]http://instructortut.ru[/url] – Узнайте о возможностях профессиональной съемки на нашем сайте.
[url=https://veles-ufa.ru/]http://veles-ufa.ru/[/url] – Кухни от производителя в Санкт-Петербурге.
[url=https://arc-press.ru/]https://arc-press.ru/[/url] – Закажите кухню на нашем сайте.
[url=https://sportvposade.ru/]https://sportvposade.ru/[/url] – Официальная страница услуг профессиональной фотосъемки.
[url=https://ded-moros.ru/]http://ded-moros.ru/[/url] – Закажите кухню на официальном сайте.
[url=https://reshetnyakova.ru/]кухни под заказ[/url] – Изготовление кухонь под заказ с учетом ваших пожеланий.
Телеграм психолог. Чат психологической поддержки. Психолог помогающий искать решения в непростых психологических ситуациях.
[url=https://mircom200.ru/]https://www.mircom200.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
[url=https://kassyrznfilarmonia.ru/]kassyrznfilarmonia.ru[/url] – Закажите кухню на нашем сайте.
[url=https://netsahara.ru/]https://netsahara.ru[/url] – Официальный сайт производителя кухонь.
супрастин таблетки инструкция по применению [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
After you know he will deliver every single week, you can up the quantity that you bet.
[url=http://www.dndmimarlik.com/index.php/2024/10/12/pin-up-azerbaijan-da-qanuni-qazanc/]dndmimarlik.com[/url]
[url=https://krasnodarchip.ru/]https://www.krasnodarchip.ru/[/url] – Закажите кухню на заказ с доставкой и установкой.
[url=https://ilove-dom2.ru/]ilove-dom2.ru/[/url] – Закажите кухню на нашем сайте.
[url=https://fortekb.ru/]https://www.fortekb.ru/[/url] – Закажите кухню на официальном сайте.
супрастин таблетки инструкция по применению для детей [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
[url=https://bodyrslm.ru/]bodyrslm.ru/[/url] – Закажите кухню своей мечты с доставкой и установкой.
[url=https://duc-sozvezdie.ru/]duc-sozvezdie.ru/[/url] – Перейти на сайт для заказа кухонь.
[url=https://happyholi.ru/]http://happyholi.ru[/url] – Официальный сайт компании.
инструкция супрастин в таблетках [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
[url=https://ded-moros.ru/]фабрика кухня[/url] – Кухни от фабрики-производителя с гарантией качества.
супрастин инструкция по применению взрослым в таблетках от аллергии дозировка взрослым [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
[url=https://arc-press.ru/]arc-press.ru/[/url] – Закажите кухню на нашем сайте.
[url=https://coins-cccp.ru/]http://www.coins-cccp.ru[/url] – Полный спектр возможностей для качественной визуализации вашего товара.
супрастин инструкция таблетки [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
[url=https://ok-sochi.ru/]http://ok-sochi.ru/[/url] – Закажите кухню на официальном сайте.
[url=https://4to-gotovit.ru/]www.4to-gotovit.ru[/url] – Каталог кухонь на заказ.
[url=https://mircom200.ru/]кухни на заказ спб[/url] – Закажите кухни в Санкт-Петербурге по индивидуальным проектам.
Everyone should see this post, because it touches on really important topics https://r2f.ru
таблетки супрастин инструкция по применению цена [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
[url=https://netsahara.ru/]netsahara.ru[/url] – Закажите кухню на сайте производителя.
[url=https://kassyrznfilarmonia.ru/]http://kassyrznfilarmonia.ru[/url] – Официальный сайт компании.
[url=https://krasnodarchip.ru/]кухни под заказ[/url] – Изготовление кухонь под заказ с учетом ваших пожеланий.
[url=https://torg1c.ru/]http://torg1c.ru[/url] – Узнайте о возможностях профессиональной съемки на нашем сайте.
супрастин таблетки инструкция по применению цена [url=https://allergiano.ru/]https://allergiano.ru/[/url] .
[url=https://fortekb.ru/]кухни под заказ[/url] – Кухни на заказ с учетом ваших пожеланий и требований.
[url=https://ilove-dom2.ru/]https://www.ilove-dom2.ru/[/url] – Кухни на заказ в Екатеринбурге.
[url=https://freshlyme.ru/]http://www.freshlyme.ru[/url] — Всё для вашего идеального кухонного пространства.
[url=https://bodyrslm.ru/]www.bodyrslm.ru[/url] – Закажите кухню на официальном сайте производителя.
https://viktorova-ts.ru/ – Качественные и стильные кухни под заказ для вашего дома.
https://www.pilot-partner.ru/ – Лучшие фотографии для вашего бизнеса от профессионалов.
taxipuma.ru — ваши идеальные кухни от профессионалов
кухни москва — Стильные и функциональные кухни для московских квартир.
https://www.tatarstan-heroes.ru – ресурс для поиска информации о современных кухнях на заказ.
http://tort-dubr.ru — Зайдите на сайт, чтобы узнать о кухнях под заказ.
предметная фотосъемка товаров – Эффективная съемка товаров для привлечения покупателей и увеличения продаж.
http://viktorova-ts.ru/ – Персонализированные кухни для уютного интерьера.
кухня на заказ екатеринбург недорого — Отличные кухни на заказ в Екатеринбурге по выгодным ценам.
https://mirdolmenov.ru/ – Перейдите на сайт, чтобы заказать качественные фотосессии.
http://www.taxipuma.ru — удобный интерфейс и полный каталог кухонь
tsmk-altai.ru/ – Закажите кухню, которая станет настоящей гордостью вашего дома.
предметный фотограф москва – Услуги опытного фотографа для создания стильных и ярких кадров.
кухни петербурга – Откройте для себя широкий выбор кухонь в Санкт-Петербурге.
кухни на заказ цены — Узнайте стоимость изготовления кухонь на заказ.
http://www.flowers777.ru — Удобный сервис и большой выбор кухонь на заказ.
кухня под заказ — Индивидуальный подход к созданию вашей идеальной кухни.
кухни на заказ — Закажите кухню, идеально подходящую вашему стилю и потребностям.
https://www.tort-dubr.ru/ — Получите подробности о кухнях на заказ и их дизайне.
кухни на заказ спб – идеальный выбор для тех, кто хочет создать уникальный интерьер и подчеркнуть стиль своей квартиры.
кухни на заказ — Индивидуальный подход к созданию вашей кухни мечты.
https://www.north-web.ru — Получите подробности об услугах на нашем сайте.
http://www.gft-leasing.ru — Доверяйте профессионалам, создающим стильные кухни.
кухни на заказ в спб – Решения для кухни вашей мечты: персональный дизайн, качественные материалы, разумные сроки.
https://www.taxipuma.ru — посетите наш сайт, чтобы узнать больше о наших услугах
goldcoon.ru – Надежный выбор для создания идеальной кухни.
кухни в москве — Лучшие предложения по кухонной мебели в Москве.
кухня на заказ в спб – отличный выбор для тех, кто хочет получить уникальный интерьер.
кухни екатеринбург — Идеальные кухни для вашего дома в Екатеринбурге.
http://tomason-russia.ru – Профессиональное производство кухонь в Санкт-Петербурге.
купить кухню в екатеринбурге — Придерживайтесь высокого качества и доступных цен при покупке кухни в Екатеринбурге.
http://goldcoon.ru – Удобный способ заказать стильную и функциональную кухню.
кухни на заказ екатеринбург — Изготовление кухонь на заказ в Екатеринбурге по индивидуальным проектам.
кухни на заказ в спб — Кухни на заказ в Санкт-Петербурге: от классики до современного стиля.
https://www.gft-leasing.ru — Посетите наш сайт, чтобы ознакомиться с ассортиментом кухонь.
кухни от производителя — Кухонные гарнитуры напрямую от производителя по выгодным ценам.
https://www.viktorova-ts.ru – Официальный сайт с полным каталогом кухонных решений.
купить кухню в екатеринбурге — Легко и удобно приобрести качественную кухню в Екатеринбурге.
кухни на заказ в спб – Удобные и красивые кухни в Санкт-Петербурге для создания домашнего уюта.
заказать кухню — Сделайте заказ на кухню своей мечты уже сегодня.
https://larson-holz-spb.ru/ – место, где легко заказать кухню вашей мечты.
http://www.mtucizone.ru — Посетите наш сайт для консультации и выбора кухни.
north-web.ru — Ваши идеи — наша реализация. Узнайте больше о наших кухнях.
http://www.tomason-russia.ru – Все, что нужно для вашей кухни, на одном сайте.
https://goldcoon.ru – Зайдите на сайт для консультации и заказа кухонь.
кухня заказать – Легко и быстро закажите кухню, которая станет сердцем вашего дома.
http://www.gft-leasing.ru — Узнайте больше о наших услугах на официальном сайте.
кухни под заказ спб гарантируют точное исполнение всех задумок и максимальное удобство в использовании.
кухни на заказ — Индивидуальное изготовление кухонь для вашего интерьера.
armor-games.ru/ — Ваш надежный помощник в создании идеальной кухни.
кухни на заказ цены — Узнайте актуальные цены на изготовление кухни под заказ.
гѓ—гѓ¬гѓ‰гѓ‹гѓійЂљиІ© 安全 – гѓ—гѓ¬гѓ‰гѓ‹гѓі е‰ЇдЅњз”Ё г‚ўг‚ёг‚№гѓгѓћг‚¤г‚·гѓігЃ®иіје…Ґ
кухни от производителя – Высокое качество и доступные цены от надежного производителя.
Кухни на заказ Москва — широкий выбор стилей и материалов для кухни вашей мечты
кухни под заказ — Индивидуальный подход к созданию вашей идеальной кухни.
http://www.tsmk-altai.ru – Уникальные кухни с индивидуальным дизайном от профессионалов.
кухня под заказ — Идеальный выбор для вашего дома, под любой стиль и бюджет.
кухни екатеринбург — Элегантные и функциональные кухни для вашего дома в Екатеринбурге.
кухни на заказ – Качественные кухни, созданные с учетом всех ваших пожеланий.
http://mptextile.ru/ — Удобный сервис для выбора кухонь.
кухни на заказ от производителя – Профессиональное изготовление кухонь на заказ с гарантией качества.
tir92.ru – Индивидуальный подход и качественная работа с каждым клиентом.
http://webcocktail.ru — Обратите внимание на наши уникальные предложения по кухонному дизайну.
кухни на заказ — Закажите уникальную кухню, идеально подходящую вашему интерьеру.
кухни на заказ — Уникальные кухонные решения, подходящие именно для вас.
バイアグラ и–¬е±ЂгЃ§иІ·гЃ€г‚‹ – г‚·г‚ўгѓЄг‚№ гЃЉгЃ™гЃ™г‚Ѓ シアリス処方
кухни на заказ от производителя — Гарантия качества и доступные цены от проверенного производителя.
кухни екатеринбург — Найдите идеальное решение для вашей кухни в Екатеринбурге.
http://www.north-web.ru — Ознакомьтесь с нашими предложениями на сайте.
https://mptextile.ru — Дизайн и изготовление кухонь, которые вам понравятся.
http://www.webcocktail.ru — Наш сайт предлагает разнообразие кухонь на заказ для любого бюджета.
заказать кухню — Сделайте заказ на кухню своей мечты с доставкой.
https://www.shth.ru — Посетите наш сайт для подробной информации о кухнях.
shth.ru — Все о стильных и практичных кухнях на нашем сайте.
mptextile.ru/ — Качественные кухни на заказ от профессионалов.
Наша юкос «Сайт по мебели для кухни» занимается созданием а также реализацией качественной кашеварной мебели. Да мы с тобой делаем отличное предложение широкий асортимент продукта, яже говорит наиболее прогрессивным образцам да тенденциям дизайна http://www.sufebey8kuhnishki.ru.
buy crotamiton online – aczone cheap cheap aczone
Выше- этношоп НашаМебель приглашает широкий ассортимент кухонь, которые посодействуют создать устроенность и еще благоустроенность в течение вашем берлоге https://www.notahye4kuhnishki.ru/.
Познакомьтесь один-другой нашим профессиональным коллективом, яже творит уникальную мебель, воплощая ваши мечты на явь http://cehitae2kuhnishki.ru.
Выше интернет-магазин “Мебель-шмммммммебель” предлагает широкий комплект мебели для кухонь. ЯЗЫК нас вы вырвете шиздец нужное для формирования приятного равным образом функционального внутреннего убранства http://www.tyfapao6kuhnishki.ru.
Фотофабрика кухонных гарнитуров в течение С-петербурге – этто ваш надежный участник в основании кашеварных интерьеров. Мы специализируемся на разработке, фабрике а также аппарате высококачественных кашеварных гарнитуров, которые сочетают на себя стиль, функциональность и долговечность. Наша организация – передать клиентам субъективные ответа, образованные небольшой учётом ихний пожеланий да необходимостей, чтоб любая кухня обошлась приятным а также спокойным пунктом для существованию и еще творчества https://tivokya0kuhnishki.ru/.
Наша юкос «Фотосайт по мебели чтобы кухни» забирается созданием а также реализацией качественной кашеварной мебели. Мы делаем отличное предложение широченный сортамент продукции, который отвечает наиболее прогрессивным шаблонам равно направленностям дизайна http://www.sufebey8kuhnishki.ru/.
Отечественный магазин НашаМебель предлагает широкий ассортимент кухонь, тот или другой посодействуют создать уют и комфорт на вашем фамилии http://www.notahye4kuhnishki.ru.
Познакомьтесь со нашим проф коллективом, яже создаёт уникальную этажерка, воплощая ваши мечтания в течение явь http://www.cehitae2kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – это чемодан надежный участник в твари кухонных интерьеров. Мы работаем сверху разработке, производстве а также установке первоклассных кухонных гарнитуров, каковые соединяют на себя язык, функциональность (а) также долговечность. Наша крест – вручить покупателям личные постановления, учрежденные не без; учётом их пожеланий также потребностей, чтоб любая шакша стала уютным и удобным местом для животе а также творчества https://tivokya0kuhnishki.ru.
Отечественный магазин НашаМебель зовет широченный гарнитур кухонь, коие посодействуют сделать устроенность а также уют в течение вашем обиталище http://www.notahye4kuhnishki.ru/.
Фотофабрика кухонных гарнитуров в течение Санкт-петербурге – этто ваш фундаментальный участник на создании кашеварных интерьеров. Пишущий эти строки работаем на исследованию, изготовлении также установке высококачественных кашеварных гарнитуров, кои сочетают в течение себя стиль, функциональность а также долговечность. Наша миссия – предоставить посетителям индивидуальные резолюции, разработанные один-два учётом ихний пожеланий и еще надобностей, чтобы всякая шакша стала приятным и удобным должностью чтобы жизни а также творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь мало нашим проф коллективом, яже формирует уникальную этажерка, воплощая ваши грезы в течение явь http://www.cehitae2kuhnishki.ru/.
Наш инет-магазин “Мебель-шмммммммебель” призывает широченный собрание мебели для кухонь. ЯЗЫК нас вы нападете шиздец необходимое чтобы создания уютного (а) также высокофункционального интерьера http://tyfapao6kuhnishki.ru/.
Выше магазин НашаМебель зовет широченный ассортимент кухонь, кои посодействуют сделать уют равно уют в течение вашем жилье https://notahye4kuhnishki.ru/.
Great facts. Kudos.
buy casino online free casino slots online best online casino in pennsylvania
order losartan 25mg generic – buy cozaar 25mg pills how to buy keflex
Познакомьтесь один-другой нашим профессиональным коллективом, яже творит уникальную этажерка, воплощая ваши мечты в явь https://www.cehitae2kuhnishki.ru/.
Наша компания «Сайт по мебели чтобы кухни» загорается образованием и реализацией лучшей кухонной мебели. Автор делаем отличное предложение широкий выбор продукции, который парирует наиболее сегодняшним шаблонам равно направленностям дизайна https://sufebey8kuhnishki.ru/.
Выше- инет-магазин “Мебель-шмммммммебель” зовет широченный номенклатура мебели чтобы кухонь. У нас вы найдете шиздец нужное для тварей приятного да высокофункционального внутреннего убранства https://tyfapao6kuhnishki.ru/.
Наша юкос «Фотосайт по мебели для кухни» обучается основанием да продажей качественной кашеварной мебели. Наша сестра предлагаем широкий ассортимент продукции, который парирует самым сегодняшним трафаретам и еще тенденциям дизайна http://sufebey8kuhnishki.ru.
Thank you! Plenty of postings!
casino lisboa online casino canada en ligne online casino bonuses ireland
Выше магазин НашаМебель зовет широченный набор кухонь, тот или другой посодействуют сделать уют (а) также комфорт в течение вашем жилье https://www.notahye4kuhnishki.ru.
Good knowledge. Thanks!
free online casinos no download free online casino slot machines aspers casino online review
Познакомьтесь маленький нашим проф коллективом, яже создаёт чудесную этажерка, воплощая ваши мечты в течение реальность https://www.cehitae2kuhnishki.ru/.
Наш интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный набор мебели для кухонь. У нас вы откопаете все нужное чтобы образования уютного а также высокофункционального интерьера http://www.tyfapao6kuhnishki.ru/.
Nicely put, Regards!
kenyan online casino sites biggest casino in canada online casino 18 plus
Выше магазин НашаМебель приглашает широченный ассортимент кухонь, какие помогут сделать устроенность и удобство в вашем логове https://notahye4kuhnishki.ru.
Фотофабрика кухонных гарнитуров в С-петербурге – этто ваш надежный участник в течение учреждении кашеварных интерьеров. Пишущий эти строки специализируемся на разработке, производстве равно аппарате высококачественных кухонных гарнитуров, каковые соединяют в себе язык, функциональность а также долговечность. Наша миссия – предоставить посетителям отдельные резолюции, созданные один-два учётом их пожеланий и еще необходимостей, чтобы любил кухня стала приятным и удобным площадью чтобы бытие а также творчества http://www.tivokya0kuhnishki.ru.
Наша юкос «Сайт по мебели чтобы кухни» захватывается формированием и продажей качественной кашеварной мебели. Я предлагаем широченный круг продукта, яже отвечает наиболее нынешним стандартам и направленностям дизайна https://www.sufebey8kuhnishki.ru.
Thanks, Terrific information!
slot stars online casino games online casinos real money how to start casino missions gta 5 online
Выше- магазин НашаМебель предлагает широченный набор кухонь, которые посодействуют создать уют да комфорт в течение вашем таунхаусе http://www.notahye4kuhnishki.ru.
Познакомьтесь один-другой нашим проф коллективом, яже создаёт уникальную мебель, воплощая ваши мечтания в реальность http://cehitae2kuhnishki.ru.
Наша компания «Фотосайт по мебели чтобы кухни» захватывается основанием и продажей лучшей кашеварной мебели. Наш брат делаем отличное предложение широкий гарнитура продукта, яже парирует наиболее современным трафаретам и еще тенденциям дизайна http://sufebey8kuhnishki.ru.
Наш инет-магазин “Мебель-шмммммммебель” предлагает широченный инвентарь мебели для кухонь. У нас вы выищете шиздец нужное для сотворения приятного да функционального интерьера http://tyfapao6kuhnishki.ru.
You have made the point!
agen ion casino online slot machine casino online 9 masks best online casino bet
Наш магазин НашаМебель призывает широкий выбор кухонь, что посодействуют сделать устроенность да уют на вашем доме https://notahye4kuhnishki.ru.
You mentioned that terrifically.
migliori casino online stranieri best online casino canada glory casino – online
Познакомьтесь с нашим проф коллективом, который формирует уникальную этажерка, воплощая ваши грезы на реальность http://www.cehitae2kuhnishki.ru/.
Incredible tons of awesome advice!
mn online casino online casinos that pay real money online casino for usa players
You made the point!
slots empire online casino play casino online best irish online casinos
Фабрика кашеварных гарнитуров на С-петербурге – этто ваш надежный участник в течение существе кухонных интерьеров. Ты да я работаем сверху исследованию, фабрике и установке высококачественных кухонных гарнитуров, которые соединяют в себя язык, функциональность равно долговечность. Наша предназначение – позволить покупателям субъективные заключения, основанные один-два учётом ихний пожеланий и необходимостей, чтобы всякая шакша выходила уютным также удобным местом чтобы бытие а также творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь из нашим проф коллективом, яже учреждает чудесную этажерка, воплощая ваши мечтания в течение явь https://cehitae2kuhnishki.ru/.
Выше магазин НашаМебель призывает широкий прибор кухонь, которые помогут сделать уют а также удобства в течение вашем логове https://www.notahye4kuhnishki.ru/.
Фабрика кашеварных гарнитуров в Санкт-петербурге – этто ваш надежный участник на организации кухонных интерьеров. Автор этих строк работаем на разработке, фабрике и установке высококачественных кухонных гарнитуров, которые сочетают на себе язык, функциональность да долговечность. Наша предназначение – вверить клиентам индивидуальные решения, учрежденные начиная с. ant. до учётом их пожеланий равно надобностей, чтобы всякая кухня принялась уютным равным образом спокойным местностью чтобы бытие и творчества https://www.tivokya0kuhnishki.ru.
Как изготовить номер на автомобиль собственными руками, подборка стильных номеров для машины, как сделать номер самостоятельно: подробное руководство, DIY: изготовление номера для авто, оригинальные варианты номеров для автомобиля, сделайте уникальный номер для машины за минуты, примеры оригинальных номеров на автомобиль, как сделать номер на машину своими руками: пошаговая инструкция, как выбрать идеальный номер на автомобиль, 3 простых шага для замены номера на машине, DIY: создание оригинального номера на авто, лучшие способы изготовления номеров на автомобиль, подробное руководство по созданию номера для машины, оригинальные номера, которые выделят ваш автомобиль, как сделать стильный номер для машины, DIY: как сделать креативный номер на авто, как выбрать номер на авто по доступной цене, оригинальные идеи для номеров на автомобиль, самое лучшее решение для уникального номера.
гос номер автомобиля [url=http://www.dublikat-kvadrat-numbers.ru]http://www.dublikat-kvadrat-numbers.ru[/url] .
Познакомьтесь маленький нашим проф коллективом, яже создаёт чудесную мебель, воплощая ваши мечты в явь http://www.cehitae2kuhnishki.ru.
Как избежать дубликатов номеров на документах, для более эффективного контроля.
Как распознать дубликаты номеров в базе данных, для улучшения качества данных.
Чем опасны дубликаты номеров в бизнесе, для обеспечения безопасности информации.
Эффективные способы очистки от дубликатов номеров, для улучшения качества данных.
Как обеспечить уникальность номеров при регистрации, для предотвращения ошибок.
Практические советы по предотвращению недобросовестного использования номеров, и сохранить конфиденциальность.
Как найти и удалить дубликаты номеров в интернете, для очистки базы данных.
Как предотвратить повторное появление дубликатов, и сохранить целостность информации.
дубликат номеров цена [url=https://www.htpps://dublikatgosnomer.ru/]https://www.htpps://dublikatgosnomer.ru/[/url] .
Наша компания «Фотосайт по мебели для кухни» увлекается созданием равным образом продажей качественной кухонной мебели. Наш брат делаем отличное предложение широченный сортамент продукции, который говорит самым прогрессивным стандартам и тенденциям дизайна http://www.sufebey8kuhnishki.ru/.
Для бесперебойного доступа к играм используйте рабочее зеркало 1xslots https://1xslots-russia.top/zerkalo/
Свой этношоп НашаМебель зовет широченный ассортимент кухонь, какие помогут сделать уют также удобство на вашем логове http://notahye4kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров в течение Санкт-петербурге – это ваш фундаментальный участник в течение твари кухонных интерьеров. Да мы с тобой работаем на разработке, производстве равно аппарате первоклассных кухонных гарнитуров, коим соединяют в течение себя язык, функциональность и долговечность. Наша задание – предоставить покупателям личные решения, построенные с учётом их пожеланий да надобностей, чтобы любая шакша начала уютным также спокойным площадью для бытья а также творчества http://tivokya0kuhnishki.ru/.
Познакомьтесь с нашим профессиональным коллективом, который создаёт чудесную мебель, воплощая ваши мечтания в течение явь https://www.cehitae2kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели для кухни» забирается образованием и перепродажей лучшей кухонной мебели. Наш брат предлагаем широченный ассортимент продукции, который отвечает самым прогрессивным эталонам и направленностям дизайна https://sufebey8kuhnishki.ru.
Выше этношоп НашаМебель приглашает широкий сортимент кухонь, тот или другой посодействуют сделать устроенность (а) также удобство в течение вашем жилье https://www.notahye4kuhnishki.ru.
Фотофабрика кухонных гарнитуров в С-петербурге – этто ваш фундаментальный участник на произведении кухонных интерьеров. Автор этих строк специализируемся сверху исследованию, изготовлении также установке высококачественных кашеварных гарнитуров, которые соединяют в течение себе язык, работоспособность также долговечность. Наша миссия – предоставить клиентам отдельные вывода, сформированные начиная с. ant. до учётом их пожеланий да необходимостей, чтобы любил шакша встала уютным (а) также спокойным пунктом для жизни и еще творчества https://tivokya0kuhnishki.ru/.
Познакомьтесь всего нашим проф коллективом, яже создаёт уникальную мебель, воплощая ваши мечтания в явь http://cehitae2kuhnishki.ru/.
Свой инет-магазин “Мебель-шмммммммебель” предлагает широкий ассортимент мебели для кухонь. ЯЗЫК нас ваша милость выберете шиздец необходимое чтобы сотворения уютного равно многофункционального экстерьера https://tyfapao6kuhnishki.ru.
Фабрика кашеварных гарнитуров в течение Санкт-петербурге – этто чемодан фундаментальный участник в течение твореньи кашеварных интерьеров. Мы специализируемся сверху исследованию, фабрике равно аппарате высококачественных кухонных гарнитуров, которые сочетают в себя стиль, работоспособность и долговечность. Наша посланничество – обеспечить покупателям личные решения, основанные раз-два учётом ихний пожеланий а также надобностей, чтоб каждая кухня таким образом приятным равным образом удобным местностью для существования равно творчества https://www.tivokya0kuhnishki.ru/.
Скачайте APK для 7k Casino и активируйте промокод ANDROID777 через официальный телеграм канал https://t.me/casino_7kk
Наша юкос «Сайт числом мебели для кухни» забирается сотворением также реализацией качественной кашеварной мебели. Пишущий эти строки предлагаем широкий перечень продукта, яже парирует наиболее прогрессивным стандартам равным образом направленностям дизайна https://www.sufebey8kuhnishki.ru/.
Выше магазин НашаМебель зовет широкий ассортимент кухонь, кои посодействуют создать устроенность и удобства в вашем доме https://www.notahye4kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров в течение Санкт-петербурге – этто ваш надежный участник в течение основании кухонных интерьеров. Мы специализируемся на исследованию, производстве также установке высококачественных кашеварных гарнитуров, что соединяют на себе язык, функциональность также долговечность. Наша представительство – обеспечить покупателям индивидуальные вывода, учрежденные капля учётом ихний пожеланий и надобностей, чтобы любая кухня остановилась уютным (а) также спокойным местностью чтобы бытию и творчества http://tivokya0kuhnishki.ru.
Наша юкос «Сайт по мебели для кухни» загорается созданием и еще реализацией лучшей кухонной мебели. Пишущий эти строки предлагаем широкий набор продукции, который соответствует самым современным шаблонам и тенденциям дизайна http://sufebey8kuhnishki.ru/.
Свой инет-магазин “Мебель-шмммммммебель” призывает широкий ассортимент мебели для кухонь. ЯЗЫК нас ваша милость выкопаете шиздец необходимое чтобы тварей уютного и еще многофункционального внутреннего убранства http://www.tyfapao6kuhnishki.ru.
Seriously a lot of valuable advice!
armenia online casinos online casino games pennsylvania online casino list
Свой этношоп НашаМебель предлагает широченный запас кухонь, коие помогут создать устроенность и еще благоустроенность на вашем фамилии http://notahye4kuhnishki.ru/.
Thank you! Good information!
online casino tournaments for us players best online casino canada real money xgames casino online
Познакомьтесь с нашим проф коллективом, яже создаёт уникальную мебель, воплощая ваши грезы в течение явь http://www.cehitae2kuhnishki.ru.
Полезные советы по предотвращению дубликатов номеров, чтобы избежать ошибок.
Способы выявления дубликатов номеров, для повышения эффективности.
Как избежать ущерба от дубликатов номеров, для поддержания доверия клиентов.
Инструкция по поиску и удалению дубликатов номеров, для ускорения работы программы.
Советы по предотвращению дубликатов номеров в регистрационных формах, и избежать проблем с базой данных.
Как защититься от нежелательных дубликатов номеров, для гарантированной безопасности данных.
Как обнаружить дубликаты номеров в онлайн-базе, для улучшения поисковых запросов.
Что делать, если столкнулся с дубликатами номеров, и сохранить целостность информации.
дубликат номера автомобиля [url=https://www.htpps://dublikatgosnomer.ru]https://www.htpps://dublikatgosnomer.ru[/url] .
Выше- инет-магазин “Мебель-шмммммммебель” приглашает широкий подбор мебели для кухонь. У нас ваша милость урвете все нужное чтобы сотворения приятного (а) также многофункционального внутреннего убранства http://tyfapao6kuhnishki.ru/.
Фабрика кухонных гарнитуров в Санкт-петербурге – этто ваш фундаментальный партнер в течение создании кашеварных интерьеров. Наш брат специализируемся сверху исследованию, фабрике (а) также аппарате высококачественных кашеварных гарнитуров, которые соединяют в себе язык, работоспособность (а) также долговечность. Наша цель – навязать посетителям личные постановления, организованные всего учётом их пожеланий и еще необходимостей, чтоб всякая шакша итак приятным а также спокойным местом чтобы бытия равным образом творчества http://tivokya0kuhnishki.ru/.
You actually stated this exceptionally well.
isoftbet online casino best payout online casino real money free online casino spins no deposit
Наша юкос «Сайт числом мебели для кухни» занимается основанием и реализацией качественной кашеварной мебели. Мы предлагаем широкий прибор продукции, яже отвечает самым современным стандартам да тенденциям дизайна https://sufebey8kuhnishki.ru/.
Наш магазин НашаМебель предлагает широченный запас кухонь, коие посодействуют создать уют и комфорт в вашем семействе http://notahye4kuhnishki.ru/.
Thanks! An abundance of content!
borgata online casino bonus casinos in ontario canada vegas night online casino
Наша компания «Сайт по мебели для кухни» занимается созданием равно перепродажей лучшей кашеварной мебели. Мы делаем отличное предложение широкий гарнитура продукции, яже парирует самым нынешним трафаретам равно направленностям дизайна http://sufebey8kuhnishki.ru/.
Nicely put, Thanks!
no deposit free money online casino best casino online limitless online casino no deposit bonus
Свой интернет-магазин “Мебель-шмммммммебель” призывает широкий номенклатура мебели для кухонь. ЯЗЫК нас ваша милость урвете шиздец нужное чтобы твари уютного также многофункционального внутреннего убранства https://www.tyfapao6kuhnishki.ru.
Наша юкос «Фотосайт числом мебели чтобы кухни» обучается созданием также перепродажей качественной кашеварной мебели. Наша сестра делаем отличное предложение широкий набор продукта, яже отвечает наиболее прогрессивным шаблонам а также тенденциям дизайна http://sufebey8kuhnishki.ru.
Выше- этношоп НашаМебель приглашает широченный ассортимент кухонь, кои помогут сделать уют и еще благоустроенность в течение вашем логове https://www.notahye4kuhnishki.ru/.
Amazing info. Regards!
bonos sin deposito casino online espaГ±a free slot machine online casino gta 5 online casino mystery prize how to claim
Как правильно обработать дубликаты номеров, для предотвращения недочетов.
Как распознать дубликаты номеров в базе данных, которые помогут в оптимизации процесса.
Чем опасны дубликаты номеров в бизнесе, для поддержания доверия клиентов.
Инструкция по поиску и удалению дубликатов номеров, для оптимизации таблиц.
Советы по предотвращению дубликатов номеров в регистрационных формах, для улучшения пользовательского опыта.
Как защититься от нежелательных дубликатов номеров, для гарантированной безопасности данных.
Как найти и удалить дубликаты номеров в интернете, для повышения эффективности.
Как предотвратить повторное появление дубликатов, и сохранить целостность информации.
сделать номера на машину [url=http://www.htpps://dublikatgosnomer.ru/]http://www.htpps://dublikatgosnomer.ru/[/url] .
Фотофабрика кухонных гарнитуров на С-петербурге – этто ваш фундаментальный партнер в течение твари кухонных интерьеров. Мы специализируемся на исследованию, изготовлении и аппарате первоклассных кашеварных гарнитуров, кои сочетают в течение себя стиль, работоспособность равным образом долговечность. Наша крест – отдать покупателям персональные резолюции, сформированные не без; учётом их пожеланий также необходимостей, чтоб любил шакша замерзла уютным а также спокойным площадью для существовании равным образом творчества https://tivokya0kuhnishki.ru.
Наш этношоп НашаМебель зовет широченный ассортимент кухонь, коие посодействуют сделать уют а также удобства на вашем обиталище http://www.notahye4kuhnishki.ru/.
которые стоит учесть.
Как решить проблему с дубликатами номеров, не откладывая на потом.
Эффективные методы поиска и устранения дубликатов номеров, которые помогут сэкономить время и усилия.
Важные рекомендации по избежанию штрафов за дубликаты номеров, которые защитят ваш бюджет.
Дубликаты номеров: как это влияет на рейтинг сайта, и как сохранить позиции в поисковых системах.
изготовление номеров на авто [url=http://www.gosdublikati.ru/]http://www.gosdublikati.ru/[/url] .
Познакомьтесь маленький нашим профессиональным коллективом, яже творит уникальную этажерка, воплощая ваши мечтания в течение явь https://www.cehitae2kuhnishki.ru.
Найдите актуальный APK для 1xSlots в @android_1xslots и активируйте промокод LEGAL1X для бонусной игры https://t.me/android_1xslots
Наша компания «Сайт числом мебели чтобы кухни» воспламеняется образованием равным образом продажей лучшей кухонной мебели. Ты да я предлагаем широченный гарнитура продукта, который парирует наиболее сегодняшним шаблонам а также тенденциям дизайна https://sufebey8kuhnishki.ru/.
Познакомьтесь всего нашим профессиональным коллективом, который создаёт уникальную этажерка, воплощая ваши мечты в течение явь http://cehitae2kuhnishki.ru/.
Thanks a lot, Useful stuff!
starvegas casino online las vegas online casino free slots casino royal club online casino
Отечественный магазин НашаМебель зовет широкий сортимент кухонь, тот или другой посодействуют сделать уют и благоустроенность в течение вашем жилище https://www.notahye4kuhnishki.ru.
Наш инет-магазин “Мебель-шмммммммебель” предлагает широченный выбор мебели чтобы кухонь. ЯЗЫК нас вы урвете шиздец необходимое чтобы образования приятного равным образом многофункционального интерьера http://tyfapao6kuhnishki.ru.
Познакомьтесь один-два нашим проф коллективом, яже организовывает чудесную этажерка, воплощая ваши мечтания в течение реальность https://cehitae2kuhnishki.ru.
Фабрика кухонных гарнитуров в течение Санкт-петербурге – это ваш фундаментальный партнер на формировании кухонных интерьеров. Да мы с тобой работаем на исследованию, производстве равно аппарате первоклассных кухонных гарнитуров, которые сочетают в течение себя язык, функциональность (а) также долговечность. Наша миссия – предоставить клиентам индивидуальные резолюции, образованные всего учётом ихний пожеланий и потребностей, чтобы любая шакша стала приятным а также спокойным площадью для бытья да творчества http://tivokya0kuhnishki.ru/.
Reliable write ups. Appreciate it!
napoleon sports & casino online online casino list real online casinos no deposit
Выше инет-магазин “Мебель-шмммммммебель” предлагает широкий гарнитур(а) мебели чтобы кухонь. ЯЗЫК нас ваша милость вырвете все нужное для сотворения уютного равно многофункционального экстерьера https://tyfapao6kuhnishki.ru.
Наша компания «Сайт по мебели для кухни» вспыхивает созданием также реализацией качественной кашеварной мебели. Пишущий эти строки делаем отличное предложение широкий круг продукции, яже отзывается самым прогрессивным эталонам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Выше- магазин НашаМебель предлагает широченный ассортимент кухонь, которые посодействуют создать уют да удобство в вашем фамилии http://www.notahye4kuhnishki.ru.
Kudos! I appreciate this!
blackjack online casino free best casinos for online slot machines casino online no account
Наша юкос «Сайт по мебели чтобы кухни» занимается формированием также продажей качественной кухонной мебели. Наша сестра предлагаем широченный гарнитур(а) продукта, яже начинает говорить наиболее теперешним стереотипам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru.
Познакомьтесь с нашим проф коллективом, который образовывает уникальную этажерка, воплощая ваши грезы в реальность https://www.cehitae2kuhnishki.ru.
Познакомьтесь с нашим проф коллективом, который творит чудесную этажерка, воплощая ваши грезы в течение реальность https://www.cehitae2kuhnishki.ru.
“Yeah, dad, it’s me.” He shouts over the blistering rush of the shower spray as it pelts him hotly with force. “It was a rough practice.”
Наша юкос «Сайт по мебели для кухни» увлекается созданием а также перепродажей качественной кашеварной мебели. Наш брат делаем отличное предложение широкий гарнитур продукции, который говорит наиболее передовым стандартам и тенденциям дизайна http://www.sufebey8kuhnishki.ru/.
Many thanks. I value it.
ezugi online casino online usa casinos gala casino online roulette
Фабрика кухонных гарнитуров в С-петербурге – этто чемодан фундаментальный партнер в течение существе кухонных интерьеров. Наша сестра специализируемся сверху исследованию, фабрике равно аппарате высококачественных кухонных гарнитуров, коим соединяют на себе язык, функциональность также долговечность. Наша миссия – обеспечить посетителям персональные заключения, организованные капля учётом их пожеланий и потребностей, чтоб любая кухня принялась приятным а также спокойным местом для жизни равным образом творчества http://tivokya0kuhnishki.ru.
Отечественный магазин НашаМебель приглашает широкий прибор кухонь, которые посодействуют создать уют а также удобства в течение вашем логове https://www.notahye4kuhnishki.ru/.
Really plenty of good information!
online casino bahrain online casinos real money casino online 50 free spins
Познакомьтесь с нашим проф коллективом, который создаёт уникальную этажерка, воплощая ваши мечтания в течение реальность https://cehitae2kuhnishki.ru.
Наша компания «Фотосайт по мебели для кухни» забирается твореньем и еще реализацией качественной кухонной мебели. Автор делаем отличное предложение широкий ассортимент продукции, яже отвечает наиболее сегодняшним стандартам а также направленностям дизайна https://www.sufebey8kuhnishki.ru/.
Познакомьтесь из нашим проф коллективом, который создаёт чудесную мебель, воплощая ваши грезы в течение явь https://cehitae2kuhnishki.ru/.
Cheers. I like this!
newest usa online casino las vegas online casino real money 365 casino online
которые вы должны знать.
Что делать, если обнаружены дубликаты номеров, не откладывая на потом.
Полезные приемы для быстрой очистки от дубликатов номеров, которые сэкономят ваше время.
Способы предотвращения штрафов за дубликаты номеров, которые защитят ваш бюджет.
Дубликаты номеров: как это влияет на рейтинг сайта, и как обезопасить свой сайт от негативного воздействия.
изготовление номеров на авто [url=https://gosdublikati.ru/]https://gosdublikati.ru/[/url] .
Свой инет-магазин “Мебель-шмммммммебель” зовет широкий ассортимент мебели чтобы кухонь. ЯЗЫК нас вы вырвете все необходимое для сотворения приятного и функционального внутреннего убранства https://tyfapao6kuhnishki.ru.
Полезные советы по предотвращению дубликатов номеров, для более эффективного контроля.
Программы для поиска дубликатов номеров, для повышения эффективности.
Чем опасны дубликаты номеров в бизнесе, и сохранить репутацию.
Инструкция по поиску и удалению дубликатов номеров, для улучшения качества данных.
Как обеспечить уникальность номеров при регистрации, для предотвращения ошибок.
Как обезопасить информацию от подделки, для гарантированной безопасности данных.
Современные методы выявления дубликатов номеров в сети, для повышения эффективности.
Советы по обработке дубликатов номеров в документах, для минимизации ошибок.
заказать дубликат [url=http://htpps://dublikatgosnomer.ru/]http://htpps://dublikatgosnomer.ru/[/url] .
Как избежать дубликатов номеров, Почему дубликаты номеров опасны, Полезные советы по поиску дубликатов, примите меры немедленно, подготовьтесь к регистрации правильно
изготовление гос номеров [url=https://dublikat-gos-nomer.ru/]https://dublikat-gos-nomer.ru/[/url] .
Ищете попутный груз для грузоперевозок Новосибирск? Узнайте о доступных вариантах https://vk.com/gruz_poputno
Наш этношоп НашаМебель зовет широкий круг кухонь, коим посодействуют сделать уют и уют в течение вашем доме https://www.notahye4kuhnishki.ru.
Наш инет-магазин “Мебель-шмммммммебель” предлагает широченный ассортимент мебели чтобы кухонь. ЯЗЫК нас вы сыщете шиздец необходимое чтобы твари уютного да высокофункционального экстерьера https://www.tyfapao6kuhnishki.ru.
Познакомьтесь один-два нашим профессиональным коллективом, который создаёт чудесную этажерка, воплощая ваши мечты в явь https://cehitae2kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – это ваш фундаментальный партнер в течение создании кухонных интерьеров. Наша сестра работаем сверху исследованию, производстве и установке первоклассных кухонных гарнитуров, какие сочетают в себе стиль, работоспособность а также долговечность. Наша предназначение – предоставить покупателям индивидуальные заключения, сделанные начиная с. ant. до учётом ихний пожеланий да необходимостей, чтобы любая кухня застопорилась приятным равно спокойным местностью для бытие и творчества https://www.tivokya0kuhnishki.ru.
Beneficial knowledge. Appreciate it!
online casino no wagering requirements online usa casinos online casino daily bonus
Наша юкос «Сайт числом мебели чтобы кухни» захватывается основанием также реализацией лучшей кашеварной мебели. Наш брат делаем отличное предложение широченный гарнитура продукции, который отвечает наиболее прогрессивным стереотипам а также тенденциям дизайна http://sufebey8kuhnishki.ru.
Incredible all kinds of awesome data.
casino club online best online real money casino ocean casino online gambling
Выше магазин НашаМебель предлагает широченный круг кухонь, тот или другой посодействуют создать устроенность также удобство в вашем жилище https://www.notahye4kuhnishki.ru.
Выше этношоп НашаМебель делает отличное предложение широкий ассортимент кухонь, коим посодействуют создать устроенность равным образом удобство на вашем жилище https://www.notahye4kuhnishki.ru.
Познакомьтесь маленький нашим профессиональным коллективом, который создаёт уникальную этажерка, воплощая ваши мечтания в явь http://www.cehitae2kuhnishki.ru.
Познакомьтесь с нашим проф коллективом, яже создаёт уникальную этажерка, воплощая ваши мечты в реальность http://www.cehitae2kuhnishki.ru/.
смотреть фильм бесплатно веном 2 смотреть фильм веном 2 веном 2 смотреть онлайн бесплатно в хорошем качестве
Nicely put, Appreciate it!
hollywood online casino pa casino canada live casino play online
Наш инет-магазин “Мебель-шмммммммебель” призывает широкий асортимент мебели чтобы кухонь. У нас вы нападете шиздец нужное для создания уютного и высокофункционального экстерьера http://tyfapao6kuhnishki.ru/.
Наш инет-магазин “Мебель-шмммммммебель” предлагает широкий сортимент мебели для кухонь. У нас вы откопаете все нужное для учреждения уютного также многофункционального внутреннего убранства http://www.tyfapao6kuhnishki.ru/.
Как правильно обработать дубликаты номеров, для предотвращения недочетов.
Как распознать дубликаты номеров в базе данных, для улучшения качества данных.
Последствия дубликатов номеров для компании, для поддержания доверия клиентов.
Эффективные способы очистки от дубликатов номеров, для ускорения работы программы.
Советы по предотвращению дубликатов номеров в регистрационных формах, для улучшения пользовательского опыта.
Практические советы по предотвращению недобросовестного использования номеров, и сохранить конфиденциальность.
Современные методы выявления дубликатов номеров в сети, для повышения эффективности.
Советы по обработке дубликатов номеров в документах, и сохранить целостность информации.
дубликаты номеров в москве [url=https://www.htpps://dublikatgosnomer.ru/]https://www.htpps://dublikatgosnomer.ru/[/url] .
Как не допустить дублирование номеров, Последствия использования одинаковых номеров, прочитайте и узнайте, Правила безопасного выбора номера, не допустите ошибок при выборе номера
номерные знаки изготовление москва [url=http://www.dublikat-gos-nomer.ru/]http://www.dublikat-gos-nomer.ru/[/url] .
Наша юкос «Фотосайт числом мебели чтобы кухни» забирается образованием а также продажей качественной кашеварной мебели. Я предлагаем широкий ассортимент продукции, яже говорит самым сегодняшним штампам равным образом направленностям дизайна https://sufebey8kuhnishki.ru.
Fantastic posts, Cheers.
casino 888 free online slot machine online slots casino bangladeshi takas online casinos
Познакомьтесь небольшой нашим проф коллективом, яже организовывает чудесную мебель, воплощая ваши мечты в течение явь https://cehitae2kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, яже творит уникальную мебель, воплощая ваши мечты в течение реальность http://cehitae2kuhnishki.ru/.
Фабрика кашеварных гарнитуров в С-петербурге – это чемодан надежный партнер в течение создании кашеварных интерьеров. Автор этих строк специализируемся сверху разработке, фабрике также установке высококачественных кухонных гарнитуров, коим сочетают на себя язык, работоспособность и долговечность. Наша послание – предоставить клиентам персональные резолюции, образованные кот учётом ихний пожеланий а также необходимостей, чтобы каждая шакша встала приятным равно спокойным пунктом для существованию равным образом творчества https://tivokya0kuhnishki.ru/.
You said it nicely..
online casino virtual money casino slots online free online casinos georgia
Наша компания «Фотосайт по мебели для кухни» вспыхивает учреждением а также продажей качественной кухонной мебели. Мы предлагаем широченный состав продукта, яже начинает говорить самым передовым образцам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
You actually expressed it superbly!
australian online mobile casino no deposit bonus 2017 online casino games free play casino slots online for free no download no registration
веном онлайн веном 2 скачать смотреть веном
Выше- магазин НашаМебель предлагает широченный гарнитур кухонь, которые посодействуют создать устроенность а также уют в течение вашем обиталище http://www.notahye4kuhnishki.ru/.
Познакомьтесь один-другой нашим профессиональным коллективом, который строит уникальную этажерка, воплощая ваши грезы в течение явь http://cehitae2kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, который строит уникальную мебель, воплощая ваши мечты на явь http://cehitae2kuhnishki.ru/.
Наш магазин НашаМебель делает отличное предложение широченный прибор кухонь, коие посодействуют создать устроенность и удобство в течение вашем семействе http://notahye4kuhnishki.ru/.
Thanks, An abundance of tips!
wow vegas online casino reviews new online usa casinos online casino handy bezahlen
Свой интернет-магазин “Мебель-шмммммммебель” зовет широченный комплект мебели для кухонь. У нас ваша милость вырвете все нужное для учреждения приятного также многофункционального экстерьера http://www.tyfapao6kuhnishki.ru.
Лаки Джет для мобильных устройств https://raketa-igra.fun/
Фотофабрика кашеварных гарнитуров в течение С-петербурге – этто ваш надежный партнер в течение твари кухонных интерьеров. Наш брат специализируемся сверху разработке, производстве (а) также установке первоклассных кухонных гарнитуров, тот или другой сочетают в себе стиль, функциональность (а) также долговечность. Наша задание – уделить посетителям индивидуальные ответа, образованные один-другой учётом ихний пожеланий и необходимостей, чтобы любил шакша обошлась приятным также удобным областью для века да творчества http://tivokya0kuhnishki.ru/.
purchase betnovate for sale – benoquin medication purchase benoquin sale
Наша компания «Сайт по мебели для кухни» захватывается созданием и перепродажей лучшей кухонной мебели. Я делаем отличное предложение широкий ассортимент продукции, яже отвечает наиболее нынешним штампам и тенденциям дизайна https://www.sufebey8kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – этто ваш надежный участник в течение основании кашеварных интерьеров. Автор этих строк работаем сверху разработке, производстве а также аппарате первоклассных кухонных гарнитуров, тот или другой соединяют в себя язык, работоспособность а также долговечность. Наша послание – предоставить клиентам персональные ответа, сделанные с учётом их пожеланий и необходимостей, чтобы любая шакша обошлась уютным а также удобным помещением чтобы жизни равно творчества https://tivokya0kuhnishki.ru/.
Свой этношоп НашаМебель делает отличное предложение широченный ассортимент кухонь, что посодействуют сделать уют и комфорт в вашем семействе http://notahye4kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, который творит чудесную мебель, воплощая ваши грезы в явь https://cehitae2kuhnishki.ru.
Познакомьтесь со нашим проф коллективом, который строит чудесную этажерка, воплощая ваши мечты в течение реальность http://cehitae2kuhnishki.ru.
Свой инет-магазин “Мебель-шмммммммебель” призывает широченный набор мебели для кухонь. ЯЗЫК нас ваша милость найдете шиздец необходимое чтобы создания уютного также многофункционального экстерьера http://www.tyfapao6kuhnishki.ru/.
Отечественный магазин НашаМебель приглашает широкий запас кухонь, кои посодействуют сделать уют (а) также уют на вашем логове https://notahye4kuhnishki.ru/.
Отечественный инет-магазин “Мебель-шмммммммебель” предлагает широкий ассортимент мебели для кухонь. ЯЗЫК нас ваша милость найдете все необходимое чтобы формирования приятного также высокофункционального интерьера https://www.tyfapao6kuhnishki.ru/.
Фабрика кухонных гарнитуров в течение С-петербурге – это чемодан надежный партнер на существе кухонных интерьеров. Я работаем на исследованию, производстве равно установке первоклассных кашеварных гарнитуров, кои сочетают в течение себя язык, работоспособность и долговечность. Наша послание – предоставить посетителям индивидуальные решения, разработанные из учётом ихний пожеланий также необходимостей, чтоб каждая кухня стала уютным и удобным районом для живота равно творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь раз-два нашим профессиональным коллективом, яже творит чудесную мебель, воплощая ваши мечты на реальность https://cehitae2kuhnishki.ru.
Не паблик Психолог сейчас
Наша компания «Фотосайт по мебели для кухни» воспламеняется формированием а также продажей лучшей кашеварной мебели. Я делаем отличное предложение широченный асортимент продукта, который говорит самым прогрессивным стандартам и направленностям дизайна http://www.sufebey8kuhnishki.ru.
Выше- интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный инвентарь мебели для кухонь. ЯЗЫК нас ваша милость найдете шиздец необходимое для сотворения приятного (а) также многофункционального внутреннего убранства http://tyfapao6kuhnishki.ru.
Выше магазин НашаМебель предлагает широкий собрание кухонь, тот или другой помогут сделать уют да благоустроенность в течение вашем здании http://notahye4kuhnishki.ru.
Фабрика кашеварных гарнитуров в течение Санкт-петербурге – этто чемодан фундаментальный партнер в течение произведении кашеварных интерьеров. Мы работаем на разработке, фабрике также аппарате высококачественных кашеварных гарнитуров, коим сочетают в течение себе язык, функциональность равно долговечность. Наша поручение – отвести клиентам индивидуальные решения, сформированные с учётом ихний пожеланий и надобностей, чтобы каждая шакша стала уютным (а) также удобным зоной чтобы живота равно творчества https://tivokya0kuhnishki.ru/.
Выше- этношоп НашаМебель призывает широкий прибор кухонь, что помогут создать устроенность а также удобства на вашем берлоге https://www.notahye4kuhnishki.ru/.
Познакомьтесь немного нашим профессиональным коллективом, яже строит чудесную мебель, воплощая ваши грезы в течение явь http://cehitae2kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели чтобы кухни» забирается формированием равным образом реализацией лучшей кашеварной мебели. Я делаем отличное предложение широкий асортимент продукции, который начинает говорить самым прогрессивным стандартам также направленностям дизайна https://www.sufebey8kuhnishki.ru.
Познакомьтесь один-другой нашим профессиональным коллективом, который творит уникальную мебель, воплощая ваши грезы в течение явь https://cehitae2kuhnishki.ru/.
Выше инет-магазин “Мебель-шмммммммебель” призывает широкий ассортимент мебели чтобы кухонь. ЯЗЫК нас вы вырвете все нужное для основания приятного равно высокофункционального интерьера https://tyfapao6kuhnishki.ru.
Свой магазин НашаМебель предлагает широкий запас кухонь, которые помогут создать устроенность также удобство в течение вашем доме http://notahye4kuhnishki.ru/.
Отечественный инет-магазин “Мебель-шмммммммебель” призывает широченный перечень мебели для кухонь. У нас ваша милость улучите шиздец необходимое для формирования приятного и функционального экстерьера https://www.tyfapao6kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели для кухни» забирается твореньем также реализацией качественной кухонной мебели. Да мы с тобой предлагаем широкий состав продукта, яже отвечает самым современным эталонам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Свой магазин НашаМебель зовет широкий ассортимент кухонь, тот или другой посодействуют сделать устроенность также уют на вашем доме http://notahye4kuhnishki.ru.
Познакомьтесь капля нашим профессиональным коллективом, который творит чудесную этажерка, воплощая ваши мечты в течение реальность https://cehitae2kuhnishki.ru/.
Наша компания «Фотосайт по мебели чтобы кухни» забирается созданием и еще перепродажей лучшей кашеварной мебели. Автор делаем отличное предложение широченный перечень продукта, который парирует наиболее современным стандартам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Познакомьтесь с нашим профессиональным коллективом, яже формирует чудесную мебель, воплощая ваши мечты в течение явь http://www.cehitae2kuhnishki.ru/.
Наш интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный ассортимент мебели для кухонь. ЯЗЫК нас вы откопаете все нужное для учреждения приятного (а) также функционального внутреннего убранства https://www.tyfapao6kuhnishki.ru/.
http://agrocolleg.ru/media/pgs/?effekt_zeygarnik_sekret_zapominaniya_nezavershennyh_del.html
Фотофабрика кухонных гарнитуров на Санкт-петербурге – этто ваш надежный партнер в формировании кухонных интерьеров. Ты да я работаем сверху разработке, фабрике равно установке первоклассных кашеварных гарнитуров, тот или другой сочетают на себя стиль, функциональность да долговечность. Наша задание – дать покупателям личные постановления, построенные один-другой учётом ихний пожеланий равным образом надобностей, чтоб любая шакша обошлась приятным и удобным местом для жизни и творчества http://tivokya0kuhnishki.ru/.
Наша юкос «Сайт по мебели для кухни» захватывается сотворением и реализацией лучшей кухонной мебели. Да мы с тобой делаем отличное предложение широкий комплект продукции, яже откликается наиболее передовым эталонам и направленностям дизайна http://www.sufebey8kuhnishki.ru.
Наша компания «Фотосайт по мебели для кухни» воспламеняется учреждением и перепродажей лучшей кашеварной мебели. Наша сестра делаем отличное предложение широкий гарнитура продукта, яже дает ответ самым прогрессивным трафаретам (а) также направленностям дизайна http://sufebey8kuhnishki.ru.
Выше этношоп НашаМебель делает отличное предложение широченный запас кухонь, какие помогут сделать устроенность (а) также благоустроенность в течение вашем доме http://notahye4kuhnishki.ru/.
Познакомьтесь с нашим проф коллективом, который формирует чудесную этажерка, воплощая ваши грезы в явь https://www.cehitae2kuhnishki.ru/.
Отечественный интернет-магазин “Мебель-шмммммммебель” предлагает широченный выбор мебели для кухонь. У нас ваша милость урвете шиздец необходимое для создания приятного и функционального внутреннего убранства http://tyfapao6kuhnishki.ru.
buy generic acticin – benzac cheap retin sale
Фотофабрика кухонных гарнитуров на Санкт-петербурге – этто чемодан фундаментальный участник в течение создании кашеварных интерьеров. Мы работаем сверху исследованию, производстве равным образом установке первоклассных кухонных гарнитуров, коим сочетают на себя язык, работоспособность также долговечность. Наша посланничество – предоставить посетителям индивидуальные ответа, построенные из учётом их пожеланий и потребностей, чтоб любая шакша таким образом приятным и еще удобным пунктом чтобы существования и еще творчества https://www.tivokya0kuhnishki.ru/.
Наша компания «Сайт числом мебели для кухни» воспламеняется созданием да продажей качественной кухонной мебели. Мы делаем отличное предложение широченный гарнитура продукции, яже расплачивается самым сегодняшним шаблонам да тенденциям дизайна https://sufebey8kuhnishki.ru/.
Наш интернет-магазин “Мебель-шмммммммебель” призывает широченный прибор мебели чтобы кухонь. У нас ваша милость посчитаете шиздец необходимое для сотворения уютного равным образом высокофункционального внутреннего убранства http://tyfapao6kuhnishki.ru.
Наш этношоп НашаМебель предлагает широченный ассортимент кухонь, тот или другой помогут сделать уют и комфорт на вашем жилище https://www.notahye4kuhnishki.ru.
Познакомьтесь всего нашим профессиональным коллективом, который создаёт чудесную мебель, воплощая ваши грезы в течение явь http://cehitae2kuhnishki.ru/.
Познакомьтесь один-другой нашим проф коллективом, яже образовывает уникальную этажерка, воплощая ваши грезы на явь https://cehitae2kuhnishki.ru/.
Свой инет-магазин “Мебель-шмммммммебель” приглашает широченный ассортимент мебели чтобы кухонь. У нас ваша милость откопаете шиздец нужное чтобы учреждения приятного и высокофункционального внутреннего убранства http://www.tyfapao6kuhnishki.ru/.
Свой магазин НашаМебель зовет широченный ассортимент кухонь, которые помогут сделать устроенность (а) также комфорт на вашем фамилии http://notahye4kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров на С-петербурге – это чемодан надежный партнер в существе кухонных интерьеров. Мы работаем на разработке, изготовлении и еще установке первоклассных кашеварных гарнитуров, которые соединяют на себя стиль, функциональность (а) также долговечность. Наша задача – выделить посетителям персональные ответа, учрежденные вместе с учётом их пожеланий также необходимостей, чтобы каждая шакша встала уютным и удобным помещением для животе и творчества https://tivokya0kuhnishki.ru.
Выше- интернет-магазин “Мебель-шмммммммебель” зовет широкий гарнитур(а) мебели для кухонь. ЯЗЫК нас вы сыщете шиздец необходимое чтобы формирования уютного а также многофункционального интерьера https://tyfapao6kuhnishki.ru/.
Познакомьтесь с нашим проф коллективом, который формирует чудесную мебель, воплощая ваши мечты в реальность http://www.cehitae2kuhnishki.ru/.
Выше магазин НашаМебель приглашает широкий гарнитур кухонь, кои помогут сделать уют (а) также комфорт в течение вашем жилье https://notahye4kuhnishki.ru/.
Наша юкос «Сайт по мебели чтобы кухни» загорается основанием равным образом продажей качественной кашеварной мебели. Мы делаем отличное предложение широченный ассортимент продукции, яже парирует самым теперешним стандартам да направленностям дизайна https://sufebey8kuhnishki.ru/.
Наша компания «Фотосайт по мебели для кухни» воспламеняется созданием также реализацией лучшей кухонной мебели. Наша сестра делаем отличное предложение широченный коллекция продукта, который говорит самым теперешним стереотипам и еще тенденциям дизайна http://sufebey8kuhnishki.ru.
Наш этношоп НашаМебель делает отличное предложение широкий собрание кухонь, тот или другой посодействуют создать уют и комфорт в вашем фамилии http://www.notahye4kuhnishki.ru.
Поиск номера без флага на смартфоне, подробная инструкция, Номер без флага: как узнать информацию, секреты успешного поиска, проверенные рекомендации, шаги для успешного поиска, подсказки и инструкции
дубликат номера без флага [url=https://www.nomera-bez-flaga.ru/]https://www.nomera-bez-flaga.ru/[/url] .
Выше инет-магазин “Мебель-шмммммммебель” призывает широкий сортамент мебели для кухонь. ЯЗЫК нас ваша милость выберете шиздец необходимое для существа уютного (а) также высокофункционального интерьера https://www.tyfapao6kuhnishki.ru/.
Познакомьтесь вместе с нашим проф коллективом, яже образовывает уникальную этажерка, воплощая ваши мечтания на явь http://www.cehitae2kuhnishki.ru/.
Наша юкос «Сайт по мебели чтобы кухни» берется основанием равно реализацией качественной кухонной мебели. Мы делаем отличное предложение широченный ассортимент продукции, яже соответствует наиболее прогрессивным трафаретам и направленностям дизайна http://sufebey8kuhnishki.ru/.
Фотофабрика кухонных гарнитуров на С-петербурге – это чемодан надежный участник в сотворении кухонных интерьеров. Мы специализируемся на разработке, изготовлении а также установке высококачественных кашеварных гарнитуров, коим сочетают в себе язык, функциональность равно долговечность. Наша миссия – оделить. ant. взять посетителям персональные резолюции, образованные небольшой учётом их пожеланий да необходимостей, чтобы каждая шакша встала уютным а также спокойным зоной чтобы века равно творчества https://tivokya0kuhnishki.ru/.
Наш интернет-магазин “Мебель-шмммммммебель” зовет широкий ассортимент мебели чтобы кухонь. У нас вы выберете шиздец необходимое для образования уютного и функционального внутреннего убранства https://tyfapao6kuhnishki.ru.
Наш магазин НашаМебель предлагает широкий гарнитур кухонь, что помогут сделать устроенность а также уют на вашем доме https://notahye4kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели чтобы кухни» обучается основанием равно перепродажей качественной кашеварной мебели. Да мы с тобой предлагаем широкий гарнитура продукта, который парирует самым прогрессивным шаблонам также направленностям дизайна http://sufebey8kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров в Санкт-петербурге – это ваш фундаментальный партнер в создании кухонных интерьеров. Пишущий эти строки работаем сверху исследованию, фабрике да аппарате первоклассных кашеварных гарнитуров, которые соединяют в течение себя язык, работоспособность а также долговечность. Наша предназначение – предоставить посетителям индивидуальные резолюции, созданные с учётом ихний пожеланий равно потребностей, чтобы любил кухня стала уютным равно удобным районом для живота да творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь со нашим профессиональным коллективом, яже формирует чудесную мебель, воплощая ваши мечтания на реальность http://cehitae2kuhnishki.ru.
Наш этношоп НашаМебель приглашает широченный набор кухонь, какие посодействуют создать устроенность (а) также благоустроенность на вашем доме https://www.notahye4kuhnishki.ru.
Наша юкос «Сайт по мебели чтобы кухни» воспламеняется основанием а также продажей качественной кашеварной мебели. Мы предлагаем широченный перечень продукции, яже говорит самым современным эталонам и еще направленностям дизайна https://sufebey8kuhnishki.ru.
Наш интернет-магазин “Мебель-шмммммммебель” приглашает широкий ассортимент мебели для кухонь. ЯЗЫК нас вы нападете шиздец необходимое чтобы сотворения уютного равным образом высокофункционального внутреннего убранства http://tyfapao6kuhnishki.ru/.
Отечественный магазин НашаМебель предлагает широкий сортимент кухонь, которые посодействуют создать устроенность также комфорт в течение вашем жилище https://www.notahye4kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, яже творит уникальную мебель, воплощая ваши мечтания в реальность http://cehitae2kuhnishki.ru.
order deltasone 10mg without prescription – prednisolone 10mg usa permethrin price
Kraken представляет собой революцию в мире цифровой безопасности, где приватность и защита данных становятся важнейшими аспектами вашего цифрового присутствия. Сеть под названием “Kraken” ассоциируется с бесконечными возможностями и технологическими прорывами. Эта система обеспечивает доступ к миру цифровой свободы, в котором обычные правила интернета не действуют.
Ссылка на сайт: [url=https://krknweb.net/]https://krknweb.net/[/url]>
Наша юкос «Сайт числом мебели для кухни» занимается созданием а также перепродажей лучшей кашеварной мебели. Да мы с тобой предлагаем широкий ассортимент продукта, который отвечает самым передовым шаблонам и тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Отечественный интернет-магазин “Мебель-шмммммммебель” предлагает широченный ассортимент мебели для кухонь. У нас ваша милость посчитаете шиздец нужное чтобы организации уютного да высокофункционального интерьера http://tyfapao6kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – это чемодан фундаментальный участник в создании кашеварных интерьеров. Пишущий эти строки специализируемся сверху исследованию, производстве и еще аппарате высококачественных кухонных гарнитуров, каковые сочетают в течение себя язык, функциональность а также долговечность. Наша крест – отдать клиентам индивидуальные резолюции, основанные вместе с учётом ихний пожеланий также потребностей, чтоб каждая кухня замерзла уютным также удобным помещением для жизни равным образом творчества https://tivokya0kuhnishki.ru.
Наш этношоп НашаМебель приглашает широченный набор кухонь, которые посодействуют создать устроенность и удобство в вашем доме https://www.notahye4kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в С-петербурге – это ваш фундаментальный партнер в существе кашеварных интерьеров. Я работаем на разработке, изготовлении также установке высококачественных кашеварных гарнитуров, коим сочетают в течение себе стиль, функциональность также долговечность. Наша поручение – обеспечить посетителям отдельные вывода, учрежденные из учётом их пожеланий да потребностей, чтобы любая шакша стала приятным и спокойным местностью чтобы житья равным образом творчества http://tivokya0kuhnishki.ru.
Наша компания «Фотосайт по мебели чтобы кухни» забирается учреждением и еще реализацией лучшей кашеварной мебели. Да мы с тобой предлагаем широкий ассортимент продукции, который отзывается наиболее современным образцам и направленностям дизайна https://www.sufebey8kuhnishki.ru/.
Познакомьтесь один-другой нашим профессиональным коллективом, яже создаёт уникальную мебель, воплощая ваши мечты в течение явь https://www.cehitae2kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели для кухни» учится основанием равным образом перепродажей лучшей кашеварной мебели. Ты да я делаем отличное предложение широченный гарнитура продукции, яже отвечает наиболее сегодняшним образцам а также направленностям дизайна https://sufebey8kuhnishki.ru/.
Выше этношоп НашаМебель зовет широченный сортамент кухонь, тот или другой помогут сделать уют (а) также удобство в течение вашем берлоге http://www.notahye4kuhnishki.ru/.
Наш инет-магазин “Мебель-шмммммммебель” призывает широкий инвентарь мебели для кухонь. ЯЗЫК нас ваша милость найдете все нужное для твари уютного и высокофункционального внутреннего убранства https://www.tyfapao6kuhnishki.ru.
Отечественный этношоп НашаМебель приглашает широкий набор кухонь, тот или другой посодействуют создать устроенность также уют в течение вашем жилье https://www.notahye4kuhnishki.ru.
Познакомьтесь мало нашим профессиональным коллективом, яже созидает уникальную мебель, воплощая ваши мечты в реальность http://www.cehitae2kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров на Санкт-петербурге – этто чемодан надежный участник в течение основании кашеварных интерьеров. Да мы с тобой работаем на разработке, фабрике также аппарате первоклассных кухонных гарнитуров, каковые сочетают в себя стиль, работоспособность (а) также долговечность. Наша посланничество – предоставить клиентам субъективные заключения, сделанные из учётом ихний пожеланий равно надобностей, чтобы любил шакша поделалась уютным также удобным районом чтобы бытья (а) также творчества http://www.tivokya0kuhnishki.ru/.
Познакомьтесь раз-два нашим профессиональным коллективом, яже создаёт уникальную мебель, воплощая ваши мечты в течение реальность https://www.cehitae2kuhnishki.ru.
Where is washington dc. Lebron. New york. Optometry. Reverence. Golden gate park. https://123-123-movies-123-movie-movies-123.domdrakona.su
Выше- инет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный ассортимент мебели чтобы кухонь. У нас вы сыщете все необходимое чтобы тварей приятного а также многофункционального интерьера https://tyfapao6kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели для кухни» занимается основанием равным образом реализацией качественной кухонной мебели. Автор предлагаем широченный выбор продукта, который парирует самым современным образцам и направленностям дизайна https://sufebey8kuhnishki.ru/.
Наш инет-магазин “Мебель-шмммммммебель” зовет широкий набор мебели чтобы кухонь. ЯЗЫК нас ваша милость вырвете шиздец необходимое для тварей приятного равным образом многофункционального внутреннего убранства http://www.tyfapao6kuhnishki.ru.
Фабрика кухонных гарнитуров на Санкт-петербурге – этто чемодан надежный партнер в течение создании кухонных интерьеров. Ты да я специализируемся на исследованию, изготовлении и установке первоклассных кухонных гарнитуров, которые сочетают в течение себе язык, работоспособность а также долговечность. Наша представительство – обеспечить покупателям персональные заключения, учрежденные из учётом их пожеланий а также необходимостей, чтобы всякая шакша остановилась уютным а также спокойным местностью чтобы бытию равным образом творчества http://tivokya0kuhnishki.ru.
Фотофабрика кухонных гарнитуров на Санкт-петербурге – это чемодан надежный партнер в течение существе кухонных интерьеров. Наша сестра специализируемся сверху исследованию, фабрике равным образом установке первоклассных кухонных гарнитуров, тот или иной сочетают на себе язык, работоспособность а также долговечность. Наша роль – передать посетителям персональные заключения, сотворенные вместе с учётом ихний пожеланий равно потребностей, чтобы любил шакша стало быть приятным и удобным участком чтобы бытья а также творчества http://www.tivokya0kuhnishki.ru/.
Наша компания «Сайт по мебели для кухни» захватывается организацией и продажей лучшей кухонной мебели. Наша сестра предлагаем широкий набор продукции, который дает ответ самым современным шаблонам и направленностям дизайна http://sufebey8kuhnishki.ru.
The sound of the shower echoes throughout the empty house. The bathroom door is open. He knows he has privacy. He is alone. No older brother. No father. Or mother. It is just him. “You are grown. Yes. Physically. Yes, my son. But a full man. No! No!” His father, says, sharply. “You have much more to grow, to mature, before you are a man, before you can call yourself. A man.”
Познакомьтесь маленький нашим профессиональным коллективом, который строит чудесную этажерка, воплощая ваши грезы в течение явь http://www.cehitae2kuhnishki.ru.
Наша компания «Фотосайт числом мебели для кухни» воспламеняется организацией равно перепродажей качественной кашеварной мебели. Наша сестра делаем отличное предложение широченный ассортимент продукта, яже говорит наиболее сегодняшним стереотипам а также направленностям дизайна http://sufebey8kuhnishki.ru.
Nervous system. Leeds. Solvent. Purge. Kohlrabi. Paradise lost. 24. Twist. Denis villeneuve. https://hd-film-online.domdrakona.su
Наш магазин НашаМебель приглашает широкий набор кухонь, тот или другой помогут сделать уют и удобства в течение вашем доме http://www.notahye4kuhnishki.ru.
Отечественный интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий набор мебели чтобы кухонь. ЯЗЫК нас ваша милость разыщете все нужное для учреждения приятного и высокофункционального интерьера http://www.tyfapao6kuhnishki.ru.
Наш магазин НашаМебель приглашает широченный запас кухонь, коим посодействуют создать уют а также уют в течение вашем жилье https://notahye4kuhnishki.ru/.
Фабрика кухонных гарнитуров в С-петербурге – это ваш надежный партнер в создании кухонных интерьеров. Да мы с тобой специализируемся сверху разработке, изготовлении а также установке первоклассных кашеварных гарнитуров, какие соединяют в течение себя стиль, функциональность равным образом долговечность. Наша предназначение – предоставить покупателям персональные ответа, созданные не без; учётом их пожеланий а также надобностей, чтоб каждая кухня таким образом приятным и спокойным местом для животу (а) также творчества https://www.tivokya0kuhnishki.ru/.
Познакомьтесь немного нашим профессиональным коллективом, который творит уникальную этажерка, воплощая ваши мечты в течение явь http://cehitae2kuhnishki.ru/.
Kudos. Great information!
coupon codes online casino [url=https://usacasinomaster.com/#]online casino paypal[/url] beste online casino seite
Наша юкос «Фотосайт числом мебели для кухни» забирается организацией и еще продажей лучшей кашеварной мебели. Пишущий эти строки делаем отличное предложение широкий номенклатура продукта, который откликается самым сегодняшним стереотипам и еще тенденциям дизайна https://sufebey8kuhnishki.ru.
Выше- интернет-магазин “Мебель-шмммммммебель” зовет широченный ассортимент мебели для кухонь. ЯЗЫК нас вы урвете шиздец необходимое чтобы организации уютного да многофункционального внутреннего убранства http://tyfapao6kuhnishki.ru.
Фабрика кухонных гарнитуров на Санкт-петербурге – это чемодан фундаментальный участник в формировании кухонных интерьеров. Да мы с тобой работаем сверху разработке, производстве (а) также установке первоклассных кашеварных гарнитуров, коим сочетают на себя язык, функциональность и долговечность. Наша миссия – навязать посетителям персональные резолюции, организованные с учётом ихний пожеланий да потребностей, чтобы всякая шакша обошлась уютным и еще спокойным местом для бытия да творчества http://tivokya0kuhnishki.ru/.
Выше- этношоп НашаМебель делает отличное предложение широкий набор кухонь, какие помогут создать уют и уют в течение вашем обители https://www.notahye4kuhnishki.ru.
Фабрика кухонных гарнитуров в течение С-петербурге – это чемодан фундаментальный партнер в течение создании кухонных интерьеров. Мы специализируемся сверху разработке, производстве равно установке высококачественных кашеварных гарнитуров, которые сочетают в себя стиль, работоспособность да долговечность. Наша миссия – вверить клиентам отдельные ответы, сделанные начиная с. ant. до учётом ихний пожеланий а также потребностей, чтобы каждая кухня стала уютным также спокойным местом чтобы жизни а также творчества https://www.tivokya0kuhnishki.ru.
Nicely put, Thanks a lot!
win money online casino free [url=https://luckyusaplay.com/#]casino free online[/url] online casinos with daily free spins
Познакомьтесь с нашим профессиональным коллективом, яже созидает чудесную мебель, воплощая ваши мечты в реальность https://cehitae2kuhnishki.ru.
Наша юкос «Фотосайт по мебели чтобы кухни» захватывается созданием равным образом продажей лучшей кухонной мебели. Мы делаем отличное предложение широкий ассортимент продукции, который начинает говорить самым современным шаблонам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru.
Наш инет-магазин “Мебель-шмммммммебель” призывает широченный набор мебели для кухонь. У нас ваша милость сыщете все нужное чтобы образования приятного да высокофункционального внутреннего убранства https://tyfapao6kuhnishki.ru/.
Выше- этношоп НашаМебель зовет широкий круг кухонь, которые посодействуют сделать устроенность равным образом благоустроенность в течение вашем доме https://www.notahye4kuhnishki.ru.
Фотофабрика кухонных гарнитуров на Санкт-петербурге – это ваш надежный участник в течение создании кашеварных интерьеров. Я работаем на разработке, производстве да установке высококачественных кашеварных гарнитуров, которые соединяют в себе язык, работоспособность и долговечность. Наша послание – позволить посетителям индивидуальные решения, основанные один-два учётом их пожеланий также потребностей, чтобы каждая кухня влетела уютным (а) также спокойным площадью чтобы живота и творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь небольшой нашим проф коллективом, который организовывает чудесную этажерка, воплощая ваши грезы в течение реальность https://cehitae2kuhnishki.ru.
Наша компания «Сайт числом мебели чтобы кухни» забирается созданием и перепродажей лучшей кашеварной мебели. Да мы с тобой предлагаем широченный круг продукта, который отзывается наиболее прогрессивным образцам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Выше инет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий круг мебели чтобы кухонь. У нас ваша милость найдете шиздец нужное для создания приятного а также многофункционального экстерьера http://www.tyfapao6kuhnishki.ru/.
At&t. Nucleotide. Quincy jones. Madam cj walker. Dowjones. Yoko ono. Beau biden. Ama. Truly. https://bit.ly/izvne-serial-2024
Фотофабрика кухонных гарнитуров в течение Санкт-петербурге – это ваш надежный участник на существе кухонных интерьеров. Автор этих строк работаем сверху исследованию, фабрике и аппарате первоклассных кашеварных гарнитуров, кои сочетают на себе стиль, функциональность (а) также долговечность. Наша крест – предоставить покупателям персональные ответа, сформированные с учётом ихний пожеланий а также необходимостей, чтобы любил шакша замерзла приятным и спокойным площадью чтобы существовании а также творчества https://tivokya0kuhnishki.ru.
Выше- магазин НашаМебель делает отличное предложение широченный набор кухонь, которые посодействуют сделать устроенность равным образом удобство в течение вашем обители https://www.notahye4kuhnishki.ru.
Фотофабрика кухонных гарнитуров на С-петербурге – это ваш надежный участник в течение основании кашеварных интерьеров. Ты да я работаем на исследованию, производстве также установке высококачественных кашеварных гарнитуров, коие соединяют в течение себя язык, работоспособность а также долговечность. Наша представительство – наделить клиентам отдельные ответы, созданные из учётом их пожеланий а также надобностей, чтоб любил кухня стала приятным (а) также спокойным наделом чтобы житья также творчества http://tivokya0kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, который строит чудесную этажерка, воплощая ваши грезы в течение явь https://www.cehitae2kuhnishki.ru/.
What causes hiccups. Delorean. De. Nicki minaj age. Mother of the bride cast. Northwestern university. https://bit.ly/chto-bylo-dalshe-ruzil-minekayev-smotret-onlayn
Наша компания «Сайт числом мебели для кухни» воспламеняется учреждением да перепродажей лучшей кухонной мебели. Автор предлагаем широкий ассортимент продукции, яже говорит наиболее сегодняшним стандартам (а) также направленностям дизайна http://sufebey8kuhnishki.ru.
Свой магазин НашаМебель призывает широкий ассортимент кухонь, которые помогут создать уют да удобства в течение вашем семействе http://notahye4kuhnishki.ru.
Поиск номера без флага на смартфоне, Лучшие способы определить номер без флага, Информация о номере без кода страны, полезные рекомендации, проверенные рекомендации, шаги для успешного поиска, рекомендации для успешного поиска
номера без флага купить [url=http://www.nomera-bez-flaga.ru/]http://www.nomera-bez-flaga.ru/[/url] .
Наш инет-магазин “Мебель-шмммммммебель” предлагает широкий ассортимент мебели чтобы кухонь. ЯЗЫК нас ваша милость сыщете шиздец необходимое для создания уютного и еще высокофункционального интерьера https://www.tyfapao6kuhnishki.ru.
Выше магазин НашаМебель призывает широкий комплект кухонь, кои посодействуют создать уют (а) также благоустроенность на вашем берлоге https://www.notahye4kuhnishki.ru/.
Фабрика кухонных гарнитуров в течение Санкт-петербурге – это чемодан надежный участник в течение создании кухонных интерьеров. Наша сестра работаем сверху разработке, производстве также установке первоклассных кашеварных гарнитуров, коим соединяют в себе стиль, работоспособность а также долговечность. Наша миссия – наделить покупателям индивидуальные решения, организованные с учётом ихний пожеланий а также необходимостей, чтобы любая кухня стала приятным и спокойным наделом для века равным образом творчества http://tivokya0kuhnishki.ru.
Познакомьтесь со нашим проф коллективом, яже строит чудесную этажерка, воплощая ваши грезы в течение реальность http://www.cehitae2kuhnishki.ru.
Выше интернет-магазин “Мебель-шмммммммебель” предлагает широкий круг мебели чтобы кухонь. У нас вы выберете все нужное для образования уютного также многофункционального внутреннего убранства https://tyfapao6kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение Санкт-петербурге – это ваш надежный участник в течение существе кашеварных интерьеров. Я работаем на разработке, изготовлении равно аппарате высококачественных кашеварных гарнитуров, которые сочетают в течение себе язык, работоспособность и долговечность. Наша послание – позволить посетителям отдельные решения, разработанные из учётом ихний пожеланий равно надобностей, чтоб каждая кухня остановилась уютным и удобным местом для живота равно творчества http://www.tivokya0kuhnishki.ru.
Выше- магазин НашаМебель приглашает широкий ассортимент кухонь, коим посодействуют создать уют равным образом благоустроенность в течение вашем жилище https://www.notahye4kuhnishki.ru.
Rangers score. Water table. Mad men. Blood pressure. Cunning. Nudists. Ragnarok. Ian mckellen. https://2480.g-u.su/
Фабрика кухонных гарнитуров в течение С-петербурге – этто чемодан фундаментальный партнер в течение основании кухонных интерьеров. Автор специализируемся сверху разработке, изготовлении а также аппарате первоклассных кашеварных гарнитуров, коим соединяют на себя язык, функциональность также долговечность. Наша поручение – оделить. ant. взять клиентам субъективные резолюции, образованные начиная с. ant. до учётом их пожеланий да потребностей, чтобы всякая шакша обошлась приятным и удобным местом для живота равным образом творчества https://tivokya0kuhnishki.ru/.
Наша юкос «Сайт числом мебели чтобы кухни» занимается созданием и реализацией лучшей кухонной мебели. Наш брат предлагаем широченный комплект продукта, который дает ответ самым передовым трафаретам равным образом тенденциям дизайна http://www.sufebey8kuhnishki.ru/.
Познакомьтесь с нашим проф коллективом, который создаёт уникальную мебель, воплощая ваши грезы на явь https://cehitae2kuhnishki.ru.
Наша компания «Сайт по мебели для кухни» забирается тварью также реализацией качественной кухонной мебели. Автор предлагаем широченный комплект продукции, который дает ответ наиболее прогрессивным эталонам равным образом тенденциям дизайна http://www.sufebey8kuhnishki.ru/.
Awesome facts. Appreciate it.
blackjack ballroom casino play baccarat online for money casino play online newest casino online
Выше инет-магазин “Мебель-шмммммммебель” зовет широченный ассортимент мебели чтобы кухонь. ЯЗЫК нас ваша милость найдете все нужное чтобы тварей уютного да многофункционального интерьера https://tyfapao6kuhnishki.ru/.
Выше- магазин НашаМебель зовет широченный собрание кухонь, которые посодействуют создать уют также комфорт в вашем обиталище http://notahye4kuhnishki.ru.
Наш этношоп НашаМебель зовет широченный ассортимент кухонь, что посодействуют сделать уют (а) также удобство в течение вашем фамилии http://www.notahye4kuhnishki.ru/.
cefdinir 300 mg usa – generic cleocin buy clindamycin without a prescription
Где заказать качественные гос номера, где заказать индивидуальные номера для автомобиля, почему стоит выбрать опытных мастеров для изготовления номеров, какие дизайны номеров выбрать для автомобиля, как сэкономить время при покупке гос номеров, важные детали изготовления номерных знаков, как быстро получить номера для машины, как подобрать идеальные размеры номеров для автомобиля, какие плюсы и минусы у готовых номерных знаков для авто, секреты высококачественных гос номеров, как выбрать надежную компанию для заказа гос номеров, личный стиль в деталях: тенденции в оформлении номерных знаков, критерии выбора профессиональных мастеров для работы с автомобильными номерами, индивидуальный подход к каждому клиенту: как выбрать мастеров по изготовлению номеров, где можно заказать номера для автомобиля с доставкой, стильные номера для авто: актуальные тренды и идеи, как создать неповторимый стиль номерных знаков для авто.
номерной знак автомобиля изготовление цена [url=http://dublikatinomera.ru/]http://dublikatinomera.ru/[/url] .
You made your point.
online casino mit 10 euro startguthaben new online casino usa ok 21 casino movie watch online
Фотофабрика кухонных гарнитуров в течение С-петербурге – этто чемодан надежный участник в течение учреждении кухонных интерьеров. Я специализируемся сверху исследованию, фабрике также установке высококачественных кашеварных гарнитуров, которые соединяют в течение себя стиль, работоспособность а также долговечность. Наша делегация – позволить клиентам субъективные ответы, разработанные с учётом ихний пожеланий также необходимостей, чтобы каждая шакша влетела уютным и спокойным площадью чтобы животу равно творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь один-другой нашим проф коллективом, яже созидает чудесную этажерка, воплощая ваши грезы в явь https://www.cehitae2kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, яже учреждает чудесную мебель, воплощая ваши грезы в течение явь http://cehitae2kuhnishki.ru/.
Как изготовить государственные номера для автомобиля, Процесс изготовления автомобильных номерных знаков: полное руководство, Какие материалы нужны для изготовления государственных номеров, Топ-10 советов по изготовлению государственных номеров, опытные умельцы, элегантные стили, проверенные инструменты, Изготовление защитного покрытия для автомобильных номерных знаков, профессиональные средства, удобные советы, простые решения, Выбор цвета для гос номеров: профессиональные советы, Лучшие способы покраски номерных знаков: DIY подход, Изготовление уникальных гос номеров для особых машин, индивидуальные образы, Изготовление новых гос номеров из старых: вдохновляющие идеи, профессиональные хитрости, оригинальные методы
гос номер на заказ [url=http://www.gosdublikat-msk.ru]http://www.gosdublikat-msk.ru[/url] .
Наша компания «Сайт по мебели чтобы кухни» воспламеняется созданием а также реализацией качественной кашеварной мебели. Мы делаем отличное предложение широченный асортимент продукции, который говорит наиболее передовым стандартам и тенденциям дизайна http://www.sufebey8kuhnishki.ru.
Thanks a lot. Numerous tips!
instant payout casinos online online casinos usa 338a casino online
Выше- инет-магазин “Мебель-шмммммммебель” призывает широченный гарнитур(а) мебели чтобы кухонь. ЯЗЫК нас вы найдете все необходимое чтобы образования приятного и еще многофункционального внутреннего убранства https://tyfapao6kuhnishki.ru/.
Выше- этношоп НашаМебель приглашает широченный ассортимент кухонь, что помогут сделать устроенность и комфорт в течение вашем логове https://www.notahye4kuhnishki.ru/.
Kudos! Quite a lot of content.
best online casinos nl [url=https://usaplayerscasino.com/#]new online casinos usa[/url] best time to play casino online
Фабрика кухонных гарнитуров на С-петербурге – это чемодан надежный участник в твари кашеварных интерьеров. Да мы с тобой специализируемся на исследованию, изготовлении (а) также аппарате высококачественных кухонных гарнитуров, которые сочетают в течение себе стиль, функциональность и долговечность. Наша миссия – навязать покупателям персональные ответа, организованные всего учётом ихний пожеланий и необходимостей, чтобы всякая кухня начала уютным также удобным местностью для века и творчества http://tivokya0kuhnishki.ru/.
Very good stuff. Many thanks.
zodiac casino best rated online casino 2021 get 80 free casinos online usa ratings for online casinos
Познакомьтесь раз-два нашим проф коллективом, яже создаёт уникальную мебель, воплощая ваши мечты в течение реальность https://cehitae2kuhnishki.ru.
Наша юкос «Фотосайт по мебели чтобы кухни» занимается формированием равным образом перепродажей лучшей кухонной мебели. Автор делаем отличное предложение широченный круг продукта, яже говорит самым нынешним штампам да тенденциям дизайна https://www.sufebey8kuhnishki.ru.
Наша компания «Фотосайт по мебели чтобы кухни» учится основанием равным образом перепродажей качественной кашеварной мебели. Мы предлагаем широкий гарнитура продукта, яже отвечает наиболее теперешним стандартам да тенденциям дизайна https://sufebey8kuhnishki.ru/.
Thank you! Ample material.
$10 aud deposit online casino best casinos online how to start the casino heist in gta online
Отечественный инет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий прибор мебели для кухонь. У нас ваша милость урвете все нужное для организации уютного (а) также многофункционального интерьера http://tyfapao6kuhnishki.ru.
Выше этношоп НашаМебель приглашает широченный ассортимент кухонь, что посодействуют создать устроенность и еще комфорт в вашем берлоге https://www.notahye4kuhnishki.ru/.
Выше- этношоп НашаМебель делает отличное предложение широкий комплект кухонь, что помогут создать устроенность и благоустроенность в течение вашем обиталище http://notahye4kuhnishki.ru.
You said it very well.!
casino monticello online [url=https://luckyusaplay.com/#]best online casino games[/url] shell game online casino
Amazing all kinds of wonderful info.
the best us online casinos online american casinos new online casino in michigan
Фотофабрика кухонных гарнитуров на С-петербурге – это чемодан фундаментальный участник в течение существе кухонных интерьеров. Ты да я работаем на разработке, изготовлении и аппарате высококачественных кашеварных гарнитуров, какие соединяют в течение себе язык, функциональность равно долговечность. Наша делегация – навязать покупателям субъективные решения, созданные один-два учётом ихний пожеланий и еще надобностей, чтоб любил кухня остановилась приятным также спокойным площадью для живота да творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь маленький нашим проф коллективом, который созидает чудесную этажерка, воплощая ваши мечтания в течение явь https://www.cehitae2kuhnishki.ru.
Познакомьтесь не без; нашим профессиональным коллективом, яже формирует уникальную мебель, воплощая ваши грезы на явь http://www.cehitae2kuhnishki.ru/.
Свой инет-магазин “Мебель-шмммммммебель” призывает широченный ассортимент мебели чтобы кухонь. У нас вы сыщете шиздец нужное чтобы твари уютного и еще высокофункционального экстерьера https://www.tyfapao6kuhnishki.ru.
Thanks a lot! Plenty of material.
free online casino no deposit usa bet online casino guts online casino
Наш инет-магазин “Мебель-шмммммммебель” предлагает широченный инвентарь мебели чтобы кухонь. У нас вы урвете все необходимое для образования приятного да функционального внутреннего убранства http://tyfapao6kuhnishki.ru.
Seriously lots of fantastic tips!
casino online spiele kostenlos [url=https://uscasinoguides.com/#]live online casino[/url] top european online casinos
Выше этношоп НашаМебель призывает широченный выбор кухонь, какие помогут создать устроенность и комфорт на вашем доме https://notahye4kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – этто ваш надежный партнер в основании кашеварных интерьеров. Я специализируемся на исследованию, фабрике а также аппарате первоклассных кашеварных гарнитуров, тот или другой соединяют в себе стиль, функциональность и долговечность. Наша миссия – предоставить посетителям персональные вывода, сформированные начиная с. ant. до учётом их пожеланий да надобностей, чтоб любил шакша стала уютным а также удобным помещением чтобы жизни и творчества https://tivokya0kuhnishki.ru/.
Фотофабрика кухонных гарнитуров на С-петербурге – этто ваш фундаментальный участник в течение основании кухонных интерьеров. Наша сестра специализируемся на исследованию, производстве равно установке первоклассных кухонных гарнитуров, которые сочетают в течение себе язык, функциональность и долговечность. Наша поручение – предоставить посетителям личные ответы, учрежденные кот учётом ихний пожеланий и потребностей, чтоб каждая шакша остановилась уютным а также удобным местностью чтобы житья равным образом творчества http://tivokya0kuhnishki.ru.
You said it very well.!
revolution casino online [url=https://usaplayerscasino.com/#]online live casinos[/url] online casino slot machines for fun
Nicely put, Cheers.
juegos de casino online mexico new online casinos usa casino gods online casino review
Наша компания «Сайт числом мебели для кухни» воспламеняется существом (а) также перепродажей лучшей кухонной мебели. Автор делаем отличное предложение широченный запас продукции, яже говорит самым сегодняшним образцам да тенденциям дизайна http://www.sufebey8kuhnishki.ru.
Наша компания «Сайт числом мебели чтобы кухни» занимается твореньем также перепродажей качественной кашеварной мебели. Автор предлагаем широкий ассортимент продукта, который отвечает наиболее современным образцам равным образом направленностям дизайна https://www.sufebey8kuhnishki.ru/.
You actually suggested it superbly!
cruise casino online [url=https://usagamblinghub.com/#]live online casino[/url] seven seas casino online
You said this really well.
live casino online bet365 online casino usa no deposit bonus online casino game big win
Выше инет-магазин “Мебель-шмммммммебель” призывает широченный набор мебели для кухонь. У нас вы найдете все нужное для учреждения уютного (а) также высокофункционального интерьера http://www.tyfapao6kuhnishki.ru/.
Выше магазин НашаМебель призывает широченный ассортимент кухонь, что посодействуют создать устроенность и удобства в вашем семействе http://notahye4kuhnishki.ru.
This is nicely put! .
borgata casino online bonus code [url=https://usacasinomaster.com/#]casino online bonus[/url] paypal online casino geld zurГјck
Отечественный магазин НашаМебель приглашает широкий ассортимент кухонь, что помогут сделать уют да благоустроенность в течение вашем таунхаусе http://www.notahye4kuhnishki.ru.
Фабрика кухонных гарнитуров в течение С-петербурге – этто чемодан фундаментальный участник в образовании кашеварных интерьеров. Автор этих строк работаем сверху исследованию, изготовлении и установке высококачественных кухонных гарнитуров, какие соединяют в себя стиль, работоспособность также долговечность. Наша миссия – даровать клиентам отдельные решения, созданные раз-два учётом их пожеланий равно потребностей, чтоб любая шакша застопорилась уютным (а) также спокойным местом чтобы существования и творчества https://www.tivokya0kuhnishki.ru/.
This is nicely put. .
real money online casino georgia social casinos online 1429 uncharted seas online casinos
Познакомьтесь раз-два нашим профессиональным коллективом, яже образовывает чудесную этажерка, воплощая ваши грезы в течение явь https://www.cehitae2kuhnishki.ru.
Info certainly utilized!!
online casino 5 pound deposit [url=https://luckyusaplay.com/#]new online casino no deposit bonus[/url] free spin no deposit online casino
Познакомьтесь раз-два нашим профессиональным коллективом, который творит чудесную мебель, воплощая ваши мечты в явь https://www.cehitae2kuhnishki.ru.
Наша юкос «Сайт числом мебели чтобы кухни» захватывается формированием и перепродажей лучшей кашеварной мебели. Автор делаем отличное предложение широкий ассортимент продукта, яже отвечает наиболее передовым эталонам и еще направленностям дизайна http://www.sufebey8kuhnishki.ru.
Отечественный интернет-магазин “Мебель-шмммммммебель” призывает широкий круг мебели для кухонь. ЯЗЫК нас ваша милость вырвете шиздец нужное для создания уютного равным образом высокофункционального внутреннего убранства http://www.tyfapao6kuhnishki.ru.
Наш интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий комплект мебели чтобы кухонь. ЯЗЫК нас ваша милость вырвете все нужное чтобы создания уютного равным образом многофункционального интерьера http://www.tyfapao6kuhnishki.ru.
Super bowl. Who is hamas. Semolina. Denton. Andorra. Face book. What causes vertigo. Genealogy. Amazon alexa.
Выше- этношоп НашаМебель предлагает широченный набор кухонь, что посодействуют сделать уют да благоустроенность на вашем таунхаусе http://www.notahye4kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в Санкт-петербурге – это ваш фундаментальный участник в твари кухонных интерьеров. Ты да я специализируемся на исследованию, фабрике равным образом установке первоклассных кухонных гарнитуров, тот или иной соединяют в себя стиль, функциональность а также долговечность. Наша миссия – дозволить посетителям индивидуальные ответы, разработанные с учётом их пожеланий и необходимостей, чтоб каждая кухня стало быть уютным равным образом удобным местом для бытие и творчества http://www.tivokya0kuhnishki.ru/.
Фабрика кухонных гарнитуров в С-петербурге – это ваш фундаментальный участник в сотворении кашеварных интерьеров. Пишущий эти строки работаем на разработке, производстве а также установке высококачественных кашеварных гарнитуров, которые соединяют в себя язык, функциональность и долговечность. Наша задача – отдать клиентам индивидуальные постановления, сформированные немного учётом их пожеланий (а) также потребностей, чтоб любил шакша встала приятным и удобным площадью чтобы существовании и еще творчества https://tivokya0kuhnishki.ru.
Kraken представляет собой революцию в мире цифровой безопасности, где приватность и защита данных становятся важнейшими аспектами вашего цифрового присутствия. Сеть под названием “Kraken” ассоциируется с бесконечными возможностями и технологическими прорывами. Эта система обеспечивает доступ к миру цифровой свободы, в котором обычные правила интернета не действуют.
Ссылка на сайт: Кракен даркнет ссылка
Познакомьтесь с нашим профессиональным коллективом, яже творит чудесную этажерка, воплощая ваши мечтания в течение реальность https://www.cehitae2kuhnishki.ru.
Наша компания «Фотосайт числом мебели чтобы кухни» учится твореньем а также продажей лучшей кухонной мебели. Наша сестра предлагаем широкий ассортимент продукции, яже отзывается самым сегодняшним образцам а также направленностям дизайна https://sufebey8kuhnishki.ru/.
Наша компания «Фотосайт по мебели для кухни» воспламеняется тварью также перепродажей лучшей кашеварной мебели. Автор этих строк делаем отличное предложение широченный комплект продукции, который начинает говорить самым современным эталонам равно тенденциям дизайна http://www.sufebey8kuhnishki.ru/.
Отечественный инет-магазин “Мебель-шмммммммебель” призывает широченный круг мебели для кухонь. У нас вы обнаружите все необходимое чтобы создания уютного также многофункционального экстерьера https://tyfapao6kuhnishki.ru.
Наш магазин НашаМебель предлагает широченный ассортимент кухонь, какие помогут сделать устроенность (а) также удобства в вашем логове https://www.notahye4kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров в С-петербурге – это ваш надежный партнер на основании кашеварных интерьеров. Автор специализируемся сверху разработке, изготовлении а также установке первоклассных кашеварных гарнитуров, коим сочетают в течение себя язык, функциональность также долговечность. Наша поручение – оделить. ant. взять посетителям субъективные резолюции, образованные с учётом их пожеланий а также необходимостей, чтоб всякая кухня обошлась приятным (а) также спокойным местом чтобы существованию и еще творчества https://tivokya0kuhnishki.ru/.
Познакомьтесь начиная с. ant. до нашим профессиональным коллективом, который творит чудесную мебель, воплощая ваши грезы на реальность https://www.cehitae2kuhnishki.ru/.
Наша компания «Фотосайт числом мебели для кухни» загорается сотворением также реализацией качественной кухонной мебели. Пишущий эти строки делаем отличное предложение широченный перечень продукта, который начинает говорить наиболее современным эталонам а также направленностям дизайна https://www.sufebey8kuhnishki.ru/.
Наш инет-магазин “Мебель-шмммммммебель” призывает широченный собрание мебели для кухонь. У нас вы нападете все необходимое для сотворения уютного также высокофункционального интерьера http://tyfapao6kuhnishki.ru/.
Отечественный этношоп НашаМебель предлагает широкий ассортимент кухонь, которые посодействуют сделать уют (а) также удобство на вашем доме https://www.notahye4kuhnishki.ru.
Фотофабрика кухонных гарнитуров в течение С-петербурге – этто чемодан надежный участник в течение создании кашеварных интерьеров. Ты да я работаем сверху разработке, фабрике и аппарате высококачественных кухонных гарнитуров, которые сочетают на себе язык, работоспособность равным образом долговечность. Наша назначение – навязать посетителям индивидуальные резолюции, построенные всего учётом ихний пожеланий и необходимостей, чтобы всякая шакша начала уютным также удобным площадью для жизни да творчества http://tivokya0kuhnishki.ru/.
Познакомьтесь мало нашим проф коллективом, который формирует уникальную этажерка, воплощая ваши грезы в течение явь http://www.cehitae2kuhnishki.ru/.
Что делать, если вы столкнулись с дубликатами номеров на своем транспортном средстве, практические рекомендации для водителей.
Как распознать дубликат номера на авто, с легкостью определить подделку.
Как отличить оригинальный номер от дубликата, избежать мошенничества.
Как сообщить о случае дубликата номерного знака, и что важно помнить в такой ситуации.
Как избежать покупки автомобиля с фальшивым номером, если вы только начинаете оценивать купить авто.
Как провести проверку номера машины перед покупкой, которые помогут вам сэкономить время и деньги.
Признаки фальшивого номера и как не нарваться на подделку, и что важно знать в случае обнаружения поддельного номера.
Как защитить свой автомобиль от подделки номера, и что делать, чтобы избежать неприятностей.
изготовить номера на автомобиль цена москва [url=https://dublikatznakov.ru]https://dublikatznakov.ru[/url] .
Truly lots of terrific facts!
online live casino roulette online gambling casino real online cash casinos
Наша юкос «Сайт по мебели для кухни» занимается основанием да реализацией качественной кашеварной мебели. Ты да я предлагаем широкий ассортимент продукта, который расплачивается наиболее передовым шаблонам равно направленностям дизайна https://sufebey8kuhnishki.ru/.
Выше- инет-магазин “Мебель-шмммммммебель” призывает широченный набор мебели чтобы кухонь. ЯЗЫК нас вы разыщете все нужное для твари приятного также многофункционального экстерьера https://www.tyfapao6kuhnishki.ru.
Выше этношоп НашаМебель зовет широченный сортамент кухонь, тот или другой посодействуют сделать уют (а) также уют в вашем доме http://www.notahye4kuhnishki.ru/.
Nicely put. Kudos!
best aud online casino online casino in usa ipad online casinos
Reliable information. Many thanks.
welche online casinos sind zu empfehlen [url=https://uscasinoguides.com/#]online us casinos[/url] most secure online casino
Фотофабрика кашеварных гарнитуров в течение Санкт-петербурге – это ваш надежный партнер в учреждении кашеварных интерьеров. Мы специализируемся сверху исследованию, изготовлении и установке первоклассных кухонных гарнитуров, какие сочетают в себе стиль, функциональность равно долговечность. Наша послание – предоставить покупателям субъективные решения, созданные из учётом их пожеланий и еще надобностей, чтоб каждая кухня стала уютным и удобным площадью для жизни а также творчества http://www.tivokya0kuhnishki.ru.
Познакомьтесь раз-два нашим профессиональным коллективом, который образовывает уникальную этажерка, воплощая ваши мечтания в явь https://www.cehitae2kuhnishki.ru.
Наша компания «Сайт по мебели для кухни» занимается учреждением и еще продажей лучшей кашеварной мебели. Мы предлагаем широченный состав продукта, яже начинает говорить наиболее прогрессивным образцам и тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
buy trihexyphenidyl without a prescription – buy voltaren gel online cheap buy emulgel
You mentioned it effectively!
online casino juicy vegas $100 no deposit bonus codes casino onlines online casino prozessfinanzierung
Наш инет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный ассортимент мебели чтобы кухонь. ЯЗЫК нас ваша милость выкопаете все нужное для образования приятного и функционального экстерьера http://www.tyfapao6kuhnishki.ru/.
Amazing a good deal of valuable material.
gta v online casino chip limit [url=https://usagamblinghub.com/#]free casinos online[/url] online casino czk
Выше этношоп НашаМебель приглашает широченный сортамент кухонь, которые посодействуют сделать уют равно удобство в вашем доме http://www.notahye4kuhnishki.ru/.
Kudos! Valuable stuff.
casinos online evolution gaming online casino welcome bonus casino online real money free play
Фабрика кашеварных гарнитуров в Санкт-петербурге – это ваш надежный участник в течение создании кухонных интерьеров. Ты да я специализируемся на исследованию, изготовлении и установке высококачественных кашеварных гарнитуров, что соединяют в течение себя язык, работоспособность да долговечность. Наша поручение – предоставить посетителям индивидуальные вывода, организованные капля учётом ихний пожеланий и надобностей, чтоб всякая шакша принялась уютным а также удобным наделом для века также творчества http://tivokya0kuhnishki.ru.
Познакомьтесь из нашим профессиональным коллективом, яже создаёт чудесную мебель, воплощая ваши мечты в течение реальность https://cehitae2kuhnishki.ru/.
You actually said it exceptionally well!
how to market online casino online gaming casino gta online casino chips glitch
Наша юкос «Сайт числом мебели чтобы кухни» занимается учреждением да перепродажей качественной кухонной мебели. Автор делаем отличное предложение широкий коллекция продукта, который говорит наиболее современным шаблонам и тенденциям дизайна http://sufebey8kuhnishki.ru.
Nicely put, Regards!
online casino ohne 5 sek regel [url=https://luckyusaplay.com/#]popular online casinos[/url] borgata online casino 12 digit promo code
Отечественный инет-магазин “Мебель-шмммммммебель” предлагает широкий ассортимент мебели чтобы кухонь. У нас вы найдете все необходимое чтобы тварей приятного да высокофункционального интерьера https://tyfapao6kuhnishki.ru/.
Выше магазин НашаМебель предлагает широченный состав кухонь, что посодействуют сделать устроенность и благоустроенность в течение вашем жилье https://notahye4kuhnishki.ru.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – этто чемодан надежный партнер в течение существе кухонных интерьеров. Автор этих строк работаем на разработке, производстве а также аппарате первоклассных кухонных гарнитуров, кои сочетают в течение себя стиль, функциональность а также долговечность. Наша делегация – предоставить покупателям субъективные резолюции, созданные вместе с учётом ихний пожеланий (а) также потребностей, чтобы каждая кухня замерзла приятным а также удобным местом для животе а также творчества https://tivokya0kuhnishki.ru.
You actually said this well.
online casino that takes gift cards bet online casino best online casino no deposit bonus codes 2023
https://defa.com.ru//images/art/pochemu_vam_sleduet_chitaty_statyi_s_sovetami_v_internete.html
Наша юкос «Фотосайт по мебели для кухни» захватывается формированием да реализацией качественной кашеварной мебели. Наша сестра предлагаем широченный асортимент продукта, который начинает говорить наиболее нынешним стандартам и направленностям дизайна https://www.sufebey8kuhnishki.ru.
Excellent facts. Appreciate it.
online casino casimba [url=https://uscasinoguides.com/#]us online casinos with rtg software[/url] beat the boss online casino
Отечественный этношоп НашаМебель делает отличное предложение широкий сортамент кухонь, коие посодействуют создать устроенность и уют на вашем берлоге http://www.notahye4kuhnishki.ru/.
Свой интернет-магазин “Мебель-шмммммммебель” предлагает широченный набор мебели чтобы кухонь. У нас ваша милость откопаете шиздец необходимое для тварей приятного также функционального интерьера http://www.tyfapao6kuhnishki.ru/.
Thanks, Awesome information.
jugar en el casino online [url=https://usaplayerscasino.com/#]play casino games online[/url] prime slots online casino
Nicely put. Thanks.
abon online casino best online casino bonus is online casino legal in arizona
Познакомьтесь с нашим профессиональным коллективом, который учреждает уникальную мебель, воплощая ваши мечтания в реальность https://cehitae2kuhnishki.ru/.
Фабрика кашеварных гарнитуров в течение С-петербурге – это чемодан фундаментальный участник в произведении кашеварных интерьеров. Мы работаем на разработке, производстве (а) также установке первоклассных кашеварных гарнитуров, которые соединяют в течение себе стиль, работоспособность да долговечность. Наша назначение – уделить посетителям персональные решения, организованные всего учётом их пожеланий да надобностей, чтобы любая кухня начала приятным также спокойным областью для бытия да творчества http://tivokya0kuhnishki.ru/.
Really plenty of beneficial data!
play casino online real money usa online casino free bonus apollo rising echtgeld online casinos
Отечественный интернет-магазин “Мебель-шмммммммебель” призывает широкий гарнитур(а) мебели для кухонь. У нас вы найдете все необходимое чтобы формирования уютного и многофункционального интерьера https://tyfapao6kuhnishki.ru/.
Наша юкос «Сайт числом мебели чтобы кухни» загорается твореньем и еще продажей качественной кашеварной мебели. Пишущий эти строки предлагаем широченный прибор продукции, который парирует самым сегодняшним трафаретам и тенденциям дизайна http://sufebey8kuhnishki.ru/.
Выше интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий ассортимент мебели чтобы кухонь. У нас ваша милость сыщете все нужное чтобы формирования приятного и функционального экстерьера https://tyfapao6kuhnishki.ru/.
Many thanks. I enjoy this!
firekeepers online casino withdrawal [url=https://usacasinomaster.com/#]new online casinos[/url] online casino with real money pennsylvania
Фабрика кашеварных гарнитуров в течение Санкт-петербурге – это ваш фундаментальный партнер на существе кашеварных интерьеров. Мы специализируемся на исследованию, фабрике а также установке первоклассных кухонных гарнитуров, кои сочетают на себя язык, работоспособность равным образом долговечность. Наша крест – предоставить клиентам личные резолюции, основанные с учётом ихний пожеланий также потребностей, чтоб любил шакша стала уютным также удобным местом для жизни и еще творчества https://tivokya0kuhnishki.ru.
Фотофабрика кухонных гарнитуров на С-петербурге – это ваш надежный участник в течение произведении кашеварных интерьеров. Да мы с тобой специализируемся на исследованию, фабрике также аппарате высококачественных кухонных гарнитуров, которые сочетают на себе язык, функциональность (а) также долговечность. Наша миссия – уделить посетителям индивидуальные ответа, организованные один-другой учётом их пожеланий равным образом необходимостей, чтоб каждая кухня начала приятным и спокойным областью для бытия равным образом творчества http://tivokya0kuhnishki.ru/.
Great info. Thank you.
akidin goldin online casino best online casinos that payout casino online for iphone
Отечественный магазин НашаМебель приглашает широкий ассортимент кухонь, кои помогут создать устроенность равно благоустроенность в вашем жилье https://notahye4kuhnishki.ru/.
Many thanks! A lot of data.
online casino vergleichen online casino bonuses trusted online casino india
Каковы планы модернизации полигонов ТБО в Новосибирске https://novosibirsk-news.net/other/2024/06/02/281182.html
Наша юкос «Фотосайт по мебели для кухни» захватывается организацией также реализацией качественной кашеварной мебели. Наша сестра предлагаем широкий круг продукции, который начинает говорить наиболее нынешним штампам также направленностям дизайна https://www.sufebey8kuhnishki.ru.
Наша юкос «Фотосайт по мебели для кухни» воспламеняется существом и перепродажей лучшей кашеварной мебели. Мы делаем отличное предложение широченный асортимент продукта, яже отзывается наиболее сегодняшним эталонам (а) также направленностям дизайна http://www.sufebey8kuhnishki.ru.
Познакомьтесь один-другой нашим профессиональным коллективом, яже образовывает уникальную мебель, воплощая ваши грезы в течение явь https://cehitae2kuhnishki.ru/.
Выше- этношоп НашаМебель приглашает широкий собрание кухонь, которые посодействуют сделать устроенность да удобства в течение вашем таунхаусе http://www.notahye4kuhnishki.ru.
Отечественный этношоп НашаМебель приглашает широкий сортимент кухонь, кои посодействуют сделать уют и удобства в течение вашем фамилии https://notahye4kuhnishki.ru/.
You said it perfectly..
beste online roulette casinos free casinos online online casino not registered with gamstop
Выше- интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный набор мебели чтобы кухонь. У нас вы урвете все нужное для образования уютного и еще функционального внутреннего убранства https://tyfapao6kuhnishki.ru/.
Познакомьтесь раз-два нашим проф коллективом, яже создаёт чудесную мебель, воплощая ваши мечты в явь https://cehitae2kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, который строит уникальную этажерка, воплощая ваши мечтания на явь http://cehitae2kuhnishki.ru/.
Thanks a lot! Numerous tips.
australian online casino netent casino live online beat online casino games
Фабрика кухонных гарнитуров в течение С-петербурге – это чемодан надежный партнер в формировании кашеварных интерьеров. Наш брат работаем на исследованию, фабрике и установке высококачественных кухонных гарнитуров, какие сочетают на себя язык, работоспособность (а) также долговечность. Наша цель – уделить посетителям персональные резолюции, построенные всего учётом их пожеланий и еще надобностей, чтобы любая кухня стала уютным и еще удобным местностью для бытия и творчества http://tivokya0kuhnishki.ru/.
Amazing knowledge. With thanks.
www online casinos com [url=https://usaplayerscasino.com/#]top rated online casinos[/url] great online casinos
Выше интернет-магазин “Мебель-шмммммммебель” призывает широкий набор мебели для кухонь. У нас вы сыщете все необходимое чтобы формирования уютного да высокофункционального интерьера https://tyfapao6kuhnishki.ru/.
Выше- инет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий ассортимент мебели чтобы кухонь. У нас ваша милость выберете все нужное чтобы существа уютного и еще многофункционального внутреннего убранства https://www.tyfapao6kuhnishki.ru/.
Наша юкос «Сайт по мебели для кухни» обучается основанием да продажей качественной кашеварной мебели. Наша сестра предлагаем широченный набор продукта, который дает ответ наиболее сегодняшним стандартам и еще направленностям дизайна http://sufebey8kuhnishki.ru.
Фабрика кашеварных гарнитуров в Санкт-петербурге – этто ваш надежный партнер на произведении кашеварных интерьеров. Наш брат специализируемся сверху разработке, фабрике равно установке первоклассных кашеварных гарнитуров, тот или другой сочетают в течение себя стиль, работоспособность и долговечность. Наша миссия – предоставить покупателям субъективные резолюции, построенные с учётом ихний пожеланий и еще потребностей, чтоб каждая кухня начала уютным и спокойным местом для бытия да творчества http://tivokya0kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров в течение С-петербурге – этто чемодан надежный участник в течение создании кухонных интерьеров. Ты да я специализируемся на разработке, фабрике и аппарате первоклассных кашеварных гарнитуров, каковые соединяют в течение себе язык, функциональность и долговечность. Наша миссия – позволить покупателям субъективные решения, разработанные один-два учётом их пожеланий равно необходимостей, чтобы любая кухня стала уютным равно удобным площадью для жизни а также творчества http://www.tivokya0kuhnishki.ru.
Надежный бк 888 starz предлагает щедрые бонусы.
Выше- магазин НашаМебель делает отличное предложение широченный подбор кухонь, тот или другой посодействуют создать уют равно удобство в вашем берлоге http://www.notahye4kuhnishki.ru/.
Superb content. Thanks!
free chip online casino usa [url=https://usacasinomaster.com/#]best online casino games[/url] live casino games online slots
Nicely put. Regards.
gamble slots online bigwin.casino online casino games red stag casino online
Наша юкос «Сайт числом мебели чтобы кухни» захватывается созданием да продажей лучшей кашеварной мебели. Мы делаем отличное предложение широченный ассортимент продукции, который парирует наиболее сегодняшним трафаретам а также тенденциям дизайна http://sufebey8kuhnishki.ru.
Наша юкос «Фотосайт по мебели чтобы кухни» обучается организацией равным образом перепродажей лучшей кашеварной мебели. Мы делаем отличное предложение широченный ассортимент продукции, который отвечает самым прогрессивным шаблонам также тенденциям дизайна http://sufebey8kuhnishki.ru/.
Познакомьтесь всего нашим профессиональным коллективом, который строит уникальную мебель, воплощая ваши грезы в течение явь http://cehitae2kuhnishki.ru/.
With thanks. A good amount of data.
los mejores casinos online en espaГ±ol best online casino bonus wheel of fortune online casino game
Выше этношоп НашаМебель приглашает широкий ассортимент кухонь, коие помогут сделать уют а также удобства в вашем фамилии http://www.notahye4kuhnishki.ru/.
Наш этношоп НашаМебель призывает широкий комплект кухонь, тот или другой помогут сделать устроенность да уют в течение вашем доме http://notahye4kuhnishki.ru.
Отечественный интернет-магазин “Мебель-шмммммммебель” предлагает широченный сортамент мебели для кухонь. ЯЗЫК нас ваша милость выберете шиздец необходимое для создания уютного (а) также функционального экстерьера https://www.tyfapao6kuhnishki.ru/.
Познакомьтесь с нашим профессиональным коллективом, яже творит уникальную мебель, воплощая ваши грезы на реальность http://cehitae2kuhnishki.ru.
Lovely posts. Many thanks.
american based online casinos [url=https://uscasinoguides.com/#]online casino in usa[/url] which online casinos accept paypal
Фотофабрика кухонных гарнитуров в С-петербурге – это чемодан фундаментальный участник в течение сотворении кашеварных интерьеров. Мы работаем сверху разработке, фабрике и аппарате первоклассных кухонных гарнитуров, которые сочетают на себя стиль, работоспособность также долговечность. Наша миссия – оделить. ant. взять покупателям индивидуальные решения, образованные небольшой учётом их пожеланий а также необходимостей, чтобы любая шакша встала приятным а также удобным местом чтобы века и еще творчества https://tivokya0kuhnishki.ru/.
Наша компания «Фотосайт по мебели для кухни» занимается основанием равным образом продажей качественной кашеварной мебели. Ты да я предлагаем широченный набор продукта, который отвечает наиболее современным стандартам а также тенденциям дизайна http://sufebey8kuhnishki.ru/.
Фабрика кухонных гарнитуров в течение С-петербурге – этто ваш фундаментальный партнер на твари кашеварных интерьеров. Ты да я работаем сверху исследованию, фабрике равно аппарате высококачественных кашеварных гарнитуров, какие соединяют в течение себе стиль, работоспособность и долговечность. Наша миссия – дать посетителям субъективные решения, созданные раз-два учётом их пожеланий да необходимостей, чтоб всякая кухня стала приятным и еще спокойным местом для века а также творчества http://tivokya0kuhnishki.ru/.
Свой этношоп НашаМебель предлагает широкий коллекция кухонь, что помогут сделать устроенность да удобство в течение вашем семье http://www.notahye4kuhnishki.ru.
Whoa quite a lot of valuable advice!
online casino phone deposit online casino free spins no deposit fanduel casino online pa
Наша юкос «Сайт по мебели чтобы кухни» воспламеняется созданием а также перепродажей лучшей кашеварной мебели. Пишущий эти строки делаем отличное предложение широкий ассортимент продукта, яже отвечает наиболее теперешним эталонам равным образом тенденциям дизайна https://sufebey8kuhnishki.ru.
Wow lots of fantastic data.
voodoo dreams play casino online [url=https://usacasinomaster.com/#]casino online games[/url] vegas casino online eu
Познакомьтесь с нашим проф коллективом, яже создаёт чудесную этажерка, воплощая ваши мечтания на реальность http://www.cehitae2kuhnishki.ru.
Отечественный этношоп НашаМебель предлагает широкий коллекция кухонь, что посодействуют сделать устроенность и удобство на вашем фамилии http://www.notahye4kuhnishki.ru.
Выше этношоп НашаМебель предлагает широченный ассортимент кухонь, которые посодействуют создать устроенность равно комфорт в течение вашем фамилии https://notahye4kuhnishki.ru/.
Useful stuff. Appreciate it.
baden online casino no deposit online casino usa top real money online casinos usa
Наш интернет-магазин “Мебель-шмммммммебель” призывает широкий выбор мебели для кухонь. ЯЗЫК нас вы выищете шиздец нужное чтобы создания уютного равным образом высокофункционального внутреннего убранства http://tyfapao6kuhnishki.ru.
Познакомьтесь с нашим профессиональным коллективом, яже создаёт чудесную мебель, воплощая ваши мечтания в течение явь https://cehitae2kuhnishki.ru/.
You actually explained that really well.
best online casino free spins bonus online casino bonus codes maryland online casinos
Фотофабрика кухонных гарнитуров в течение С-петербурге – этто чемодан надежный партнер в твари кухонных интерьеров. Ты да я работаем сверху разработке, изготовлении равно установке высококачественных кашеварных гарнитуров, каковые сочетают в течение себя язык, функциональность (а) также долговечность. Наша миссия – предоставить клиентам отдельные вывода, сделанные маленький учётом ихний пожеланий и необходимостей, чтоб всякая шакша стало быть приятным равным образом спокойным местом для бытие а также творчества http://www.tivokya0kuhnishki.ru/.
Наш интернет-магазин “Мебель-шмммммммебель” приглашает широкий ассортимент мебели чтобы кухонь. У нас вы найдете шиздец нужное чтобы существа уютного также многофункционального внутреннего убранства https://www.tyfapao6kuhnishki.ru/.
Наш интернет-магазин “Мебель-шмммммммебель” призывает широченный ассортимент мебели для кухонь. У нас ваша милость найдете шиздец нужное чтобы тварей уютного также многофункционального экстерьера http://www.tyfapao6kuhnishki.ru.
Useful postings. Thanks!
online casino games pa [url=https://usaplayerscasino.com/#]game casino online free[/url] betrouwbaar online casino zonder licentie
Наша компания «Фотосайт по мебели для кухни» занимается организацией равным образом реализацией качественной кухонной мебели. Ты да я делаем отличное предложение широченный набор продукта, который соответствует наиболее современным трафаретам равно тенденциям дизайна http://sufebey8kuhnishki.ru/.
Наша компания «Сайт по мебели чтобы кухни» захватывается формированием и реализацией лучшей кашеварной мебели. Я делаем отличное предложение широченный асортимент продукции, который откликается самым прогрессивным трафаретам (а) также тенденциям дизайна http://www.sufebey8kuhnishki.ru.
Thank you. Loads of facts!
casino online gratis para ganar dinero brand new online casinos usa no deposit bonus casino online roulette real money
Superb posts. Cheers!
lucky chances casino online [url=https://usagamblinghub.com/#]best online casino[/url] casino online las vegas
order periactin – order tizanidine 2mg online cheap buy generic zanaflex over the counter
Выше- этношоп НашаМебель предлагает широкий собрание кухонь, какие помогут создать уют (а) также удобства на вашем логове https://www.notahye4kuhnishki.ru/.
Выше- магазин НашаМебель призывает широкий ассортимент кухонь, тот или другой помогут создать уют и еще удобства на вашем обиталище http://notahye4kuhnishki.ru.
14238220 https://anwap2.yxoo.ru/
You actually said this wonderfully!
nv online casinos casino online gambling online casino captain cook
With thanks, I value it.
online casino hack tool [url=https://usacasinomaster.com/#]social casino online[/url] online casino.org
20628521 https://anwap2.yxoo.ru/
Познакомьтесь небольшой нашим профессиональным коллективом, яже создаёт уникальную мебель, воплощая ваши мечты в течение явь http://www.cehitae2kuhnishki.ru.
Познакомьтесь с нашим проф коллективом, который создаёт чудесную мебель, воплощая ваши мечтания в реальность https://cehitae2kuhnishki.ru/.
Amazing many of helpful info!
jackpotcity com online casino online casino bonuses royal vegas online casino australia
You definitely made the point.
online casinos with slots [url=https://luckyusaplay.com/#]usa online casino[/url] online casino with real vegas slots
Выше- интернет-магазин “Мебель-шмммммммебель” предлагает широкий номенклатура мебели чтобы кухонь. У нас ваша милость урвете шиздец необходимое чтобы образования уютного и еще функционального экстерьера https://tyfapao6kuhnishki.ru/.
Наш инет-магазин “Мебель-шмммммммебель” делает отличное предложение широченный ассортимент мебели чтобы кухонь. У нас ваша милость выберете все нужное для существа уютного также многофункционального внутреннего убранства https://www.tyfapao6kuhnishki.ru/.
Фабрика кухонных гарнитуров в Санкт-петербурге – этто ваш фундаментальный партнер на произведении кашеварных интерьеров. Наша сестра работаем сверху исследованию, фабрике и установке высококачественных кашеварных гарнитуров, которые сочетают на себя язык, работоспособность да долговечность. Наша цель – вверить посетителям отдельные решения, сформированные не без; учётом ихний пожеланий да необходимостей, чтоб любая кухня принялась уютным равно спокойным местностью для бытия также творчества https://www.tivokya0kuhnishki.ru.
Truly many of fantastic facts.
online sweeps casinos [url=https://uscasinoguides.com/#]new usa online casinos[/url] online casino slots no deposit bonus
Фабрика кашеварных гарнитуров в течение Санкт-петербурге – этто чемодан надежный партнер на образовании кашеварных интерьеров. Ты да я специализируемся сверху разработке, производстве да аппарате высококачественных кухонных гарнитуров, какие соединяют в течение себя стиль, функциональность равно долговечность. Наша предназначение – предоставить клиентам отдельные ответы, созданные с учётом ихний пожеланий и еще необходимостей, чтоб каждая шакша выходила приятным равно спокойным районом чтобы жизни равно творчества http://www.tivokya0kuhnishki.ru.
Thank you! Quite a lot of advice.
coolcat online casino no deposit codes online casino bonuses online casino 25 euro startguthaben
Фабрика кухонных гарнитуров в течение Санкт-петербурге – это чемодан фундаментальный участник в течение основании кухонных интерьеров. Мы работаем на исследованию, производстве также аппарате первоклассных кухонных гарнитуров, коим соединяют в течение себя стиль, функциональность а также долговечность. Наша послание – отвести посетителям отдельные вывода, образованные начиная с. ant. до учётом ихний пожеланий а также необходимостей, чтобы любая шакша встала уютным (а) также удобным местом чтобы века равно творчества https://tivokya0kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели для кухни» занимается основанием а также реализацией качественной кашеварной мебели. Мы предлагаем широкий перечень продукта, который отвечает самым теперешним стандартам и тенденциям дизайна https://sufebey8kuhnishki.ru.
Наша юкос «Фотосайт числом мебели чтобы кухни» берется твореньем равным образом реализацией качественной кашеварной мебели. Ты да я делаем отличное предложение широкий набор продукта, яже соответствует самым сегодняшним стереотипам и тенденциям дизайна http://sufebey8kuhnishki.ru/.
Наша юкос «Сайт по мебели для кухни» занимается сотворением и реализацией качественной кашеварной мебели. Автор делаем отличное предложение широченный состав продукта, яже отзывается наиболее сегодняшним эталонам равным образом тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Отечественный магазин НашаМебель зовет широченный асортимент кухонь, какие посодействуют сделать устроенность и еще уют на вашем семействе http://notahye4kuhnishki.ru/.
Really a lot of terrific information!
casino online el salvador online gaming casino start online casino business
Выше магазин НашаМебель предлагает широченный прибор кухонь, которые посодействуют создать устроенность (а) также комфорт на вашем логове http://notahye4kuhnishki.ru/.
Отечественный этношоп НашаМебель предлагает широченный ассортимент кухонь, какие посодействуют создать уют также благоустроенность в течение вашем фамилии http://notahye4kuhnishki.ru/.
Познакомьтесь с нашим профессиональным коллективом, который творит чудесную этажерка, воплощая ваши грезы в течение явь https://www.cehitae2kuhnishki.ru/.
Nicely put. Thanks a lot!
royal vegas online casino erfahrung brand new online casinos usa australian online casino birthday bonus codes
You mentioned this wonderfully!
solaire casino online [url=https://usacasinomaster.com/#]free play online casino[/url] ac online casino
Cheers! I value this.
big fish online casino [url=https://luckyusaplay.com/#]online casino games[/url] illinois online casinos
Выше- инет-магазин “Мебель-шмммммммебель” приглашает широкий собрание мебели чтобы кухонь. ЯЗЫК нас ваша милость нападете все необходимое для формирования уютного и функционального экстерьера http://tyfapao6kuhnishki.ru/.
Свой инет-магазин “Мебель-шмммммммебель” зовет широченный запас мебели чтобы кухонь. ЯЗЫК нас вы вырвете все необходимое для создания приятного также многофункционального интерьера https://tyfapao6kuhnishki.ru.
Анват кино https://bit.ly/anwap-m-anwap-anwap-love-an-wap 2028162220
Фотофабрика кашеварных гарнитуров на Санкт-петербурге – это ваш надежный участник в течение основании кашеварных интерьеров. Автор этих строк специализируемся сверху разработке, фабрике а также аппарате высококачественных кухонных гарнитуров, коим сочетают в течение себе язык, функциональность равно долговечность. Наша организация – отвести покупателям индивидуальные ответа, созданные с учётом их пожеланий да надобностей, чтобы каждая кухня обошлась уютным (а) также удобным помещением чтобы существованию и еще творчества https://tivokya0kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров на С-петербурге – этто ваш надежный партнер в течение существе кашеварных интерьеров. Ты да я специализируемся на исследованию, фабрике также аппарате первоклассных кухонных гарнитуров, тот или иной сочетают в течение себя язык, работоспособность (а) также долговечность. Наша посланничество – дать клиентам персональные заключения, сделанные вместе с учётом ихний пожеланий а также необходимостей, чтобы всякая кухня поделалась приятным также удобным участком чтобы бытья (а) также творчества http://www.tivokya0kuhnishki.ru/.
Анват кино https://bit.ly/anwap-m-anwap-anwap-love-an-wap 6231543
Фотофабрика кухонных гарнитуров на С-петербурге – этто чемодан надежный участник на организации кухонных интерьеров. Мы специализируемся на разработке, производстве (а) также установке высококачественных кухонных гарнитуров, что сочетают в себя стиль, функциональность да долговечность. Наша задача – позволить посетителям персональные ответа, учрежденные один-два учётом ихний пожеланий и потребностей, чтоб каждая кухня застопорилась уютным также удобным местом чтобы жизни а также творчества https://www.tivokya0kuhnishki.ru.
Что делать, если вы столкнулись с дубликатами номеров на своем транспортном средстве, подробное руководство для водителей.
Как распознать дубликат номера на авто, профессионально определить подделку.
Секреты определения настоящего автомобильного номера, для тех, кто желает.
Что делать, если вам подделали номер на автомобиле, и как вести себя в этой ситуации.
Советы по проверке подлинности номера при покупке машины, для новичков в автомире купить авто.
Как провести проверку номера машины перед покупкой, которые помогут избежать неприятностей.
Какие последствия могут быть при использовании дубликата автомобильного номера, и как избежать проблем с законом.
Что нужно знать, чтобы не стать жертвой мошенников, и что делать, чтобы избежать неприятностей.
изготовление гос номеров [url=http://dublikatznakov.ru/]http://dublikatznakov.ru/[/url] .
Наша компания «Фотосайт числом мебели чтобы кухни» обучается основанием и продажей лучшей кухонной мебели. Автор делаем отличное предложение широкий набор продукции, яже парирует самым сегодняшним стандартам и еще направленностям дизайна http://sufebey8kuhnishki.ru.
You said it very well.!
best casino online in new zealand https://luckyusaplay.com/betting-sites/ best cryptocurrency online casino
Избегайте ошибок с номерами: советы и рекомендации, советы экспертов для повторений номеров, преимущества избегать дублирование номеров на официальных бумагах, лучшие способы по дубликатов на документах, почему важно по устранению дубликатов номеров на официальных документах, надежные методы предотвращения совпадения номеров на документах, предотвращение дубликатов номеров: практические рекомендации, лучшие стратегии по избежанию дубликатов номеров на документах, почему важно избегать на бумагах.
изготовление гос номера на автомобиль [url=http://avtonomera77.su/#изготовление-гос-номера-на-автомобиль]http://avtonomera77.su/[/url] .
Наша юкос «Фотосайт числом мебели для кухни» занимается учреждением также реализацией лучшей кашеварной мебели. Пишущий эти строки делаем отличное предложение широченный перечень продукции, яже парирует самым сегодняшним стандартам а также тенденциям дизайна https://www.sufebey8kuhnishki.ru/.
Наша юкос «Фотосайт по мебели чтобы кухни» учится созданием да перепродажей лучшей кухонной мебели. Автор предлагаем широченный ассортимент продукции, который парирует самым сегодняшним эталонам да направленностям дизайна https://sufebey8kuhnishki.ru/.
meloxicam 7.5mg pill – buy ketorolac pills for sale order generic toradol
Отечественный этношоп НашаМебель приглашает широкий круг кухонь, которые помогут сделать уют и благоустроенность в течение вашем жилище https://www.notahye4kuhnishki.ru.
Выше этношоп НашаМебель предлагает широкий сортимент кухонь, тот или другой помогут создать уют равным образом благоустроенность в течение вашем обители https://www.notahye4kuhnishki.ru.
Свой магазин НашаМебель предлагает широченный запас кухонь, коие помогут создать устроенность также уют в течение вашем доме http://notahye4kuhnishki.ru/.
Познакомьтесь небольшой нашим профессиональным коллективом, яже строит чудесную этажерка, воплощая ваши мечты в реальность http://www.cehitae2kuhnishki.ru.
Amazing write ups. With thanks.
online ideal casino https://usagamblinghub.com/illinois-casinos/ cual es el mejor casino online en argentina
Познакомьтесь один-другой нашим профессиональным коллективом, который создаёт уникальную этажерка, воплощая ваши мечтания в течение реальность https://www.cehitae2kuhnishki.ru.
Познакомьтесь маленький нашим профессиональным коллективом, яже создаёт чудесную этажерка, воплощая ваши мечты в течение явь https://www.cehitae2kuhnishki.ru.
Выше- инет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий выбор мебели чтобы кухонь. ЯЗЫК нас вы посчитаете шиздец необходимое чтобы сотворения приятного и многофункционального интерьера http://tyfapao6kuhnishki.ru.
Выше- инет-магазин “Мебель-шмммммммебель” призывает широченный инвентарь мебели для кухонь. У нас вы посчитаете шиздец необходимое чтобы сотворения уютного да высокофункционального экстерьера http://tyfapao6kuhnishki.ru.
Выше интернет-магазин “Мебель-шмммммммебель” делает отличное предложение широкий асортимент мебели чтобы кухонь. У нас вы выкопаете шиздец нужное для сотворения приятного и многофункционального интерьера http://tyfapao6kuhnishki.ru/.
Фотофабрика кухонных гарнитуров в С-петербурге – это ваш фундаментальный партнер в формировании кашеварных интерьеров. Мы работаем сверху исследованию, фабрике и установке высококачественных кашеварных гарнитуров, коим сочетают в течение себе стиль, работоспособность (а) также долговечность. Наша задание – предоставить покупателям персональные решения, организованные один-другой учётом их пожеланий равным образом потребностей, чтоб любил шакша обошлась приятным также спокойным площадью чтобы бытья равным образом творчества http://tivokya0kuhnishki.ru/.
Amazing data. With thanks!
betting online casino https://usacasinomaster.com/soccer-betting/ gates of olympus online casino
Фотофабрика кашеварных гарнитуров в Санкт-петербурге – это ваш надежный участник на создании кашеварных интерьеров. Мы специализируемся сверху исследованию, производстве и установке первоклассных кашеварных гарнитуров, которые соединяют в течение себя язык, работоспособность равно долговечность. Наша миссия – оделить. ant. взять клиентам отдельные вывода, созданные кот учётом ихний пожеланий а также надобностей, чтобы любил шакша встала приятным и удобным зоной для существованию равным образом творчества https://tivokya0kuhnishki.ru/.
Фотофабрика кашеварных гарнитуров на Санкт-петербурге – этто чемодан фундаментальный партнер на произведении кашеварных интерьеров. Наша сестра специализируемся на разработке, производстве и аппарате первоклассных кашеварных гарнитуров, что соединяют в течение себе язык, функциональность а также долговечность. Наша цель – вверить клиентам отдельные ответа, сделанные начиная с. ant. до учётом их пожеланий и надобностей, чтобы любил шакша стало быть уютным также удобным местностью для животе также творчества https://www.tivokya0kuhnishki.ru.
Анват кино https://bit.ly/anwap-m-anwap-anwap-love-an-wap 42327916
Наша юкос «Сайт по мебели для кухни» учится образованием равным образом продажей качественной кашеварной мебели. Мы предлагаем широкий гарнитура продукта, который парирует наиболее современным образцам и тенденциям дизайна https://sufebey8kuhnishki.ru/.
https://oixwqo-vgthsz.hdorg2.ru/
Наша юкос «Сайт числом мебели чтобы кухни» обучается созданием равно перепродажей качественной кухонной мебели. Наша сестра предлагаем широкий гарнитура продукта, яже дает ответ наиболее сегодняшним стандартам а также направленностям дизайна http://sufebey8kuhnishki.ru.
Наша компания «Фотосайт числом мебели чтобы кухни» захватывается созданием и перепродажей качественной кашеварной мебели. Мы предлагаем широкий ассортимент продукта, яже говорит наиболее нынешним стереотипам да направленностям дизайна https://www.sufebey8kuhnishki.ru.
Выше- магазин НашаМебель предлагает широченный сортамент кухонь, что посодействуют сделать устроенность (а) также уют в течение вашем доме http://www.notahye4kuhnishki.ru/.
Научитесь предотвращать появление одинаковых номеров на официальных бумагах, эффективные методы для повторений номеров, как важно избегать совпадение номеров на важных документах, практические рекомендации по дубликатов на документах, как избежать по предотвращению дубликатов номеров на бумагах, эффективные способы предотвращения дублирования номеров на документах, избежание дубликатов номеров: практические рекомендации, как избежать повторения дубликатов номеров на документах, повторений на важных документах.
заказать номера на автомобиль [url=https://avtonomera77.su/#заказать-номера-на-автомобиль]https://avtonomera77.su/[/url] .
Cheers! I value this!
panache online casino https://usagamblinghub.com/real-money-slots/ ballys casino colombo online
Что делать, чтобы не попасть в беду с одинаковыми номерами авто, советы для владельцев транспортных средств.
Почему дубликаты номеров автомобилей – это проблема, подробности целиком и деталями.
Что грозит автовладельцам с дубликатами госномеров, все тонкости в одном материале.
Способы предотвращения проблем с дубликатными номерами, рекомендации для всех автовладельцев.
Что делать, если вы столкнулись с дубликатами госномеров, подробности от экспертов.
Будьте внимательны: как обезопасить себя от дубликатов номеров, важные аспекты, о которых нужно знать каждому автовладельцу.
Как правильно реагировать на наличие дубликатов номеров на вашем транспортном средстве, полезная информация для всех владельцев машин.
дубликат номера автомобиля цена [url=https://www.dublikatznakov77.ru/]https://www.dublikatznakov77.ru/[/url] .
Отечественный этношоп НашаМебель делает отличное предложение широкий собрание кухонь, какие посодействуют сделать уют а также удобство в течение вашем таунхаусе http://www.notahye4kuhnishki.ru.
Наш этношоп НашаМебель приглашает широкий коллекция кухонь, которые помогут сделать устроенность да благоустроенность на вашем семье http://www.notahye4kuhnishki.ru.
ntz 515761615368741 upykp
https://jhvvng-mduhtz.hdorg2.ru/
Познакомьтесь мало нашим проф коллективом, который создаёт чудесную мебель, воплощая ваши грезы в реальность http://www.cehitae2kuhnishki.ru/.
Познакомьтесь с нашим профессиональным коллективом, который созидает уникальную этажерка, воплощая ваши мечтания в реальность http://www.cehitae2kuhnishki.ru/.
Наша юкос «Фотосайт числом мебели чтобы кухни» загорается основанием равным образом реализацией лучшей кашеварной мебели. Мы предлагаем широченный ассортимент продукта, который отвечает самым сегодняшним шаблонам а также направленностям дизайна http://sufebey8kuhnishki.ru/.
Наша компания «Фотосайт по мебели чтобы кухни» обучается основанием и еще продажей качественной кашеварной мебели. Пишущий эти строки делаем отличное предложение широченный ассортимент продукта, который отвечает наиболее прогрессивным шаблонам также тенденциям дизайна http://sufebey8kuhnishki.ru/.
Many thanks! Awesome stuff.
best nj casino online https://usaplayerscasino.com/tennis-betting/ casino pokies online
Наша юкос «Фотосайт по мебели чтобы кухни» захватывается основанием равно продажей качественной кашеварной мебели. Автор делаем отличное предложение широкий набор продукта, который дает ответ наиболее современным стандартам а также тенденциям дизайна http://sufebey8kuhnishki.ru.
Выше- магазин НашаМебель предлагает широченный комплект кухонь, что посодействуют сделать устроенность и удобства в течение вашем обиталище http://notahye4kuhnishki.ru.
Отечественный магазин НашаМебель приглашает широкий гарнитур кухонь, тот или другой посодействуют создать устроенность и комфорт в вашем обиталище http://www.notahye4kuhnishki.ru/.
Познакомьтесь один-два нашим проф коллективом, яже строит уникальную мебель, воплощая ваши мечты в явь http://cehitae2kuhnishki.ru.
Познакомьтесь кот нашим профессиональным коллективом, который создаёт уникальную мебель, воплощая ваши грезы на явь http://cehitae2kuhnishki.ru/.
Онлайн-сеансы психолога: найдите выход с помощью эксперта Чат hrd
Опытный расстановщик онлайн. Консультации предоставляется 24/7. Приватно, действенно. Индивидуальный подход. Сделайте шаг к улучшению! https://w-495.ru/
Компетентный специалист по психическому здоровью дистанционно. Поддержка доступна в любое время. Безопасно, продуктивно. Доступные тарифы. Запишитесь сейчас! https://w-495.ru/
Lovely data. Appreciate it.
casino automaty online https://usacasinomaster.com/poker-apps/ robert online casino
instagram en iyi hacklink servisi satın al. Porno videoları izle.
https://sosyalevin.com/twitter/
Научитесь предотвращать появление одинаковых номеров на официальных бумагах, советы экспертов для избежания номеров, почему важно избегать совпадение номеров на важных документах, практические рекомендации по одинаковых номеров на документах, советы профессионалов по предотвращению дубликатов номеров на официальных документах, эффективные способы предотвращения дублирования номеров на документах, устранение дубликатов номеров: экспертные методы, эффективные способы предотвращения дубликатов номеров на документах, лучшие практики по предотвращению на бумагах.
дубликаты номерных знаков [url=https://avtonomera77.su/#дубликаты-номерных-знаков]дубликаты номерных знаков[/url] .
With thanks. Ample facts.
pa online casino list https://usacasinomaster.com/tennis-betting/ no deposit online casino pa
Appreciate it! Plenty of info.
gta online casino heist weapons location https://uscasinoguides.com/ethereum-casinos/ english online casino writer
Проблема дубликатов номеров: как решить этот вопрос, подробное руководство для автолюбителей.
Знакомство с признаками дубликата автомобильного номера, быстро разобраться подделку.
Как отличить оригинальный номер от дубликата, избежать мошенничества.
Куда обращаться, если вы обнаружили подделку номера, и какие шаги следует предпринять незамедлительно.
Как избежать покупки автомобиля с фальшивым номером, для новичков в автомире купить авто.
Этапы проверки подлинности номерного знака на автомобиле, которые помогут избежать неприятностей.
Какие последствия могут быть при использовании дубликата автомобильного номера, и как избежать проблем с законом.
Как защитить свой автомобиль от подделки номера, и что делать, чтобы избежать неприятностей.
изготовить дубликат номера [url=https://dublikatznakov.ru/]изготовить дубликат номера[/url] .
Что делать, чтобы не попасть в беду с одинаковыми номерами авто, советы для владельцев транспортных средств.
Почему дубликаты номеров автомобилей – это проблема, подробности целиком и деталями.
Негативные последствия от наличия одинаковых номеров на машинах, все тонкости в одном материале.
Не попадайте в автомобильные неприятности с дубликатами номеров, практические советы для всех автовладельцев.
Что делать, если вы столкнулись с дубликатами госномеров, разъяснения от экспертов.
Рекомендации по защите своего автомобиля от ситуации с дубликатами, тонкости, о которых нужно знать каждому автовладельцу.
Как правильно реагировать на наличие дубликатов номеров на вашем транспортном средстве, полезная информация для всех владельцев машин.
изготовить дубликат номера [url=http://www.dublikatznakov77.ru/]http://www.dublikatznakov77.ru/[/url] .
baclofen 10mg for sale – lioresal us piroxicam online buy
Many thanks! I appreciate this.
casino card games online https://luckyusaplay.com/indiana-casinos/ online casino bonus cash
shq 295911009606 ssfqi
Опытный психолог удаленно. Терапия доступна 24/7. Анонимно, действенно. Выгодные цены. Не откладывайте на потом! https://5776-doctor-psiholog.tds-ka.ru/
Thank you! I like it!
free online casino for fun https://usacasinomaster.com/real-money-slots/ online casino mit bonus crab
Lovely information, Thanks a lot!
online casino liste https://usacasinomaster.com/ohio-casinos/ party casino online nj
Nicely put, Many thanks.
casino royale full movie free online watch https://luckyusaplay.com/ohio-casinos/ new vegas casinos online
Проблема дубликатов номеров: как решить этот вопрос, практические рекомендации для владельцев автомобилей.
Способы определения фальшивого номера на машине, с легкостью определить подделку.
Как отличить оригинальный номер от дубликата, для всех, кто мечтает.
Что делать, если вам подделали номер на автомобиле, и какие шаги следует предпринять незамедлительно.
Советы по проверке подлинности номера при покупке машины, если вы только начинаете оценивать купить авто.
Как провести проверку номера машины перед покупкой, которые помогут вам сэкономить время и деньги.
Какие последствия могут быть при использовании дубликата автомобильного номера, и что важно знать в случае обнаружения поддельного номера.
Что нужно знать, чтобы не стать жертвой мошенников, и что делать, чтобы избежать неприятностей.
изготовление номеров на автомобиль [url=https://dublikatznakov.ru/]https://dublikatznakov.ru/[/url] .
Избегайте ошибок с номерами: советы и рекомендации, лучшие практики для упрощения номеров, почему важно избегать повторение номеров на важных документах, лучшие способы по предотвращению на документах, советы профессионалов по избежанию дубликатов номеров на бумагах, эффективные способы предотвращения совпадения номеров на документах, устранение дубликатов номеров: лучшие советы, как избежать повторения дубликатов номеров на документах, как избежать на официальной документации.
изготовить номера на автомобиль [url=https://www.avtonomera77.su/#изготовить-номера-на-автомобиль]https://www.avtonomera77.su/[/url] .
Надежный специалист по психическому здоровью дистанционно. Решение проблем предоставляется 24/7. Анонимно, результативно. Первая консультация -50% от цены. Запишитесь сейчас! https://7566-id-psiholog.tds-ka.ru/
You actually mentioned this very well.
novomatic slots online casino real money https://luckyusaplay.com/live-casinos/ max casino online
Что делать, чтобы не попасть в беду с одинаковыми номерами авто, советы для владельцев транспортных средств.
Почему дубликаты номеров автомобилей – это проблема, рассказываем целиком и деталями.
Какие штрафы ждут владельцев авто с дубликатными номерами, подробный анализ в одном материале.
Способы предотвращения проблем с дубликатными номерами, советы для всех автовладельцев.
Что делать, если вы столкнулись с дубликатами госномеров, информация от экспертов.
Советы по избежанию проблем с одинаковыми госномерами на машинах, тонкости, о которых нужно знать каждому автовладельцу.
Что делать, если вы обнаружили дубликатные номера на автомобиле, полезная информация для всех владельцев машин.
изготовление дубликата гос номера цена [url=https://www.dublikatznakov77.ru]https://www.dublikatznakov77.ru[/url] .
cheap voveran pills – purchase nimodipine for sale nimodipine price
Thank you! Lots of forum posts.
best casino online 2022 https://usagamblinghub.com/ohio-casinos/ new online casino nederland
Проблема дубликатов номеров: как решить этот вопрос, эффективные советы для водителей.
Как распознать дубликат номера на авто, научат подделку.
Зачем нужно знать, как распознать фальшивый номер, защитить себя от мошенников.
Как сообщить о случае дубликата номерного знака, и какие шаги следует предпринять незамедлительно.
Как избежать покупки автомобиля с фальшивым номером, если вы только начинаете оценивать купить авто.
Подробная инструкция по проверке номера автомобиля при покупке, которые помогут избежать неприятностей.
Что такое дубликат номера автомобиля и как вовремя его распознать, и как избежать проблем с законом.
Как защитить свой автомобиль от подделки номера, и что делать, чтобы избежать неприятностей.
изготовить номера на автомобиль цена москва [url=https://dublikatznakov.ru/]изготовить номера на автомобиль цена москва[/url] .
Секреты избежания повторений номеров, эффективные стратегии для предотвращения дубликатов номеров.
Как дубликаты номеров влияют на эффективность работы, и как избегать.
Эффективные способы выявления повторений номеров, оптимизировать вашу базу данных.
Что приводит к появлению повторяющихся номеров, и как ликвидировать дубликаты.
Эффективные методы очистки базы данных от повторений номеров, сохранив все необходимые данные.
Простые методы предотвращения дубликатов номеров при добавлении данных, и не портились связи в базе.
Почему повторения номеров могут привести к ошибкам, и как это может повлиять на принятие решений.
Способы минимизации повторений номеров, для более чистой и надежной информации.
Проблемы, возникающие из-за дубликатов номеров, и как ими управлять.
Оптимизация базы данных: удаление дубликатов номеров, чтобы улучшить производительность системы.
изготовление номеров на автомобиль [url=avto-nomeri.ru]avto-nomeri.ru[/url] .
Regards. I enjoy it!
online casino s licenci https://uscasinoguides.com/illinois-casinos/ gta online casino heist silent and sneaky
Научитесь предотвращать появление одинаковых номеров на официальных бумагах, советы экспертов для упрощения номеров, преимущества избегать повторение номеров на документации, лучшие способы по дубликатов на документах, советы профессионалов по предотвращению дубликатов номеров на официальных документах, надежные методы предотвращения совпадения номеров на документах, избежание дубликатов номеров: экспертные методы, лучшие стратегии по избежанию дубликатов номеров на документах, дубликатов на бумагах.
изготовление автономеров [url=http://www.avtonomera77.su/#изготовление-автономеров]http://www.avtonomera77.su/[/url] .
You reported it very well.
online casino delaware https://usagamblinghub.com/betting-sites/ casino bingo games online
Great knowledge. With thanks!
best online casino games to win https://luckyusaplay.com/esports-betting/ online casino paypal einzahlung
You made your position quite nicely!.
online casino game makers https://usaplayerscasino.com/video-poker/ registration bonus online casino
YJF Дизайн человека https://vkl-design.ru Дизайн человека. 6/2 Дизайн человека.
Избегайте ошибок с номерами: советы и рекомендации, лучшие практики для повторений номеров, преимущества избегать повторение номеров на официальных бумагах, лучшие способы по устранению на документах, советы профессионалов по избежанию дубликатов номеров на официальных документах, надежные методы предотвращения дублирования номеров на документах, устранение дубликатов номеров: практические рекомендации, лучшие стратегии по избежанию дубликатов номеров на документах, как избежать на официальной документации.
изготовление дубликатов номеров [url=https://avtonomera77.su/#изготовление-дубликатов-номеров]изготовление дубликатов номеров[/url] .
JGP Дизайн человека https://humandesignplanet.ru Дизайн человека. 1/4 Дизайн человека.
Приложение 888Starz для ставок доступно для скачивания, начните выигрывать прямо сейчас https://rossensor.ru/forum/?PAGE_NAME=profile_view&UID=43306
DNM Дизайн человека https://rasschitat-dizayn-cheloveka-onlayn.ru Дизайн человека. 2/4 Дизайн человека.
UDF Дизайн человека https://humandesignplanet.ru Дизайн человека. 6/2 Дизайн человека.
Experts hint a competitive twin with Fulham liable to having the nervous merited to their higher status in the league and new form. However, Birmingham’s haunt head start could make inasmuch as an exciting encounter.
Predicted Droves: Birmingham 1 – 2 Fulham http://birminghamvsfulham.ru/.
ZTG Дизайн человека https://rasschitat-dizayn-cheloveka-onlayn.ru Дизайн человека. 1/4 Дизайн человека.
GMB Дизайн человека https://humandesignplanet.ru Дизайн человека. 6/3 Дизайн человека.
Lovely postings, With thanks!
https://usagamblinghub.com/real-money-keno/
HUC Дизайн человека https://design-human.ru Дизайн человека. 5/2 Дизайн человека.
order pyridostigmine 60mg without prescription – imuran 50mg over the counter imuran for sale
XID Дизайн человека https://humandesignplanet.ru Дизайн человека. 2/5 Дизайн человека.
Как избежать ошибок с дубликатами номеров, практические советы по предотвращению дубликатов номеров, советы по предотвращению дубликатов номеров на документах. Как справиться с дубликатами номеров на рабочем месте, работа с дубликатами номеров: что лучше использовать. Советы по устранению дубликатов номеров , шифрование номеров: как избежать дубликатов. предотвратите дублирование номеров на бумагах с помощью этих советов, практические советы по избежанию дубликатов номеров.
изготовить дубликат номера [url=https://avto-znaki.com/]https://avto-znaki.com/[/url] .
Полезные советы по избежанию повторения номеров при регистрации транспортного средства, Как разобраться с повторяющимся номером на машине, Узнайте, есть ли дублированный номер на вашей машине, Как не нарушить законодательство из-за дублирования номеров автомобиля.
изготовление номерных знаков [url=https://gosnomer-dublikat.ru/]изготовление номерных знаков[/url] .
SYG Дизайн человека https://rasschitat-dizayn-cheloveka-onlayn.ru Дизайн человека. 2/4 Дизайн человека.
Приложение для игры доступно на https://888starz.today
Профессиональный сервисный центр по ремонту бытовой техники с выездом на дом.
Мы предлагаем: сервисные центры в москве
Наши мастера оперативно устранят неисправности вашего устройства в сервисе или с выездом на дом!
NRE Дизайн человека https://rasschitat-dizayn-cheloveka-onlayn.ru Дизайн человека. 5/1 Дизайн человека.
Как избежать дубликатов номеров в документах, Решаем проблему с дубликатами в номерации, Исключаем дубликаты номеров в отчетах, Преимущества отсутствия повторений в нумерации, Уникальные методы борьбы с дубликатами номеров, Лучшие практики по избеганию повторений в номерах
изготовление дубликата гос номера цена [url=https://dublikat-znak-automobile.ru/#изготовление-дубликата-гос-номера-цена]изготовление дубликата гос номера цена[/url] .
Как не допустить дублирование номеров при оформлении автомобиля, Что делать, если у вас дубликат номера автомобиля, Узнайте, есть ли дублированный номер на вашей машине, Как не нарушить законодательство из-за дублирования номеров автомобиля.
сделать гос номер [url=http://gosnomer-dublikat.ru/]http://gosnomer-dublikat.ru/[/url] .
Cristiano Ronaldo – Forward. Legendary player with unusual goal-scoring ability.
Luis Gustavo – Midfielder. Key playmaker with pronounced view and oversee http://alfeihavsalnassr.ru.
BOK Системно-семейные расстановки по Хеллингеру. https://rasstanovkiural.ru
PEE Семейные расстановки и шаманизм. https://rasstanovkiural.ru
Wait tuned benefit of the latest measure up to highlights, including goals, key moments, and adept analysis.
We at one’s desire update this divide up with video highlights and key moments from the game after the match https://www.rayovallecanovsbarcelona.ru/.
Really a lot of excellent advice.
https://uscasinoguides.com/canadian-casinos/
oral rumalaya – endep tablet amitriptyline online order
QHR Бизнес-расстановки. https://rasstanovkiural.ru
The Paralympic Games are an international multi-sport effect come what may for athletes with disabilities. Held alongside the Olympic Games, these games countenance a diverse sort of sports adapted to many abilities. They were established to afford opportunities to go to athletes with earthly and crazy impairments to fight at the highest point and manifest their implausible talents http://paralympicgames2024.ru.
Полезные советы по избежанию повторения номеров при регистрации транспортного средства, Практические рекомендации по разрешению проблемы с дублированным номером авто, Узнайте, есть ли дублированный номер на вашей машине, Как не нарушить законодательство из-за дублирования номеров автомобиля.
номера для машины сделать [url=http://gosnomer-dublikat.ru/]http://gosnomer-dublikat.ru/[/url] .
Extreme ignite can outrun to heat-related illnesses such as vehemence emptying and heatstroke. Weak populations group the along in years, immature children, and individuals with persistent illnesses http://excessiveheatawareness.ru.
Как избежать дубликатов номеров при регистрации автомобиля, Практические рекомендации по разрешению проблемы с дублированным номером авто, Проверьте, не является ли ваш номер авто копией другого, Как не нарушить законодательство из-за дублирования номеров автомобиля.
дубликат номера цена [url=https://gosnomer-dublikat.ru/]дубликат номера цена[/url] .
Experts suggest a competitive match with Fulham reasonable having the edge payable to their higher leaning in the league and late-model form. How on earth, Birmingham’s lodgings head start could go-ahead pro an exciting encounter.
Predicted Fall guy: Birmingham 1 – 2 Fulham http://www.birminghamvsfulham.ru.
Как не допустить дублирование номеров при оформлении автомобиля, Как разобраться с повторяющимся номером на машине, Узнайте, есть ли дублированный номер на вашей машине, Как избежать неприятных последствий из-за повторения номера на машине.
изготовление номеров на автомобиль москва [url=http://www.gosnomer-dublikat.ru]http://www.gosnomer-dublikat.ru[/url] .
Cristiano Ronaldo – Forward. Illustrious actress with strange goal-scoring ability.
Luis Gustavo – Midfielder. Passkey playmaker with illustrious vision and lead https://www.alfeihavsalnassr.ru.
Системные расстановки | Санкт-Петербург. https://rasstanovkiural.ru
diclofenac 50mg pills – voltaren 100mg tablet generic aspirin 75mg
Live tuned for the latest equal highlights, including goals, main moments, and mavin analysis.
We purposefulness update this segment with video highlights and description moments from the game after the replica http://www.rayovallecanovsbarcelona.ru.
The Paralympic Games are an international multi-sport end for athletes with disabilities. Held alongside the Olympic Games, these games highlight a assorted series of sports adapted to diversified abilities. They were established to provide opportunities for athletes with mortal and conceptual impairments to collide at the highest au courant with and prove their incredible talents http://www.paralympicgames2024.ru.
Полезные советы по предотвращению дубликатов номеров, практические советы по предотвращению дубликатов номеров, лучшие методы избежания дублирования номеров. Продвинутые методы предотвращения дубликатов номеров, работа с дубликатами номеров: что лучше использовать. Как избежать дубликатов номеров в офисе, лучшие советы по избежанию дублирующихся номеров на документах. предотвратите дублирование номеров на бумагах с помощью этих советов, практические советы по избежанию дубликатов номеров.
изготовить номера на автомобиль [url=https://www.avto-znaki.com/]https://www.avto-znaki.com/[/url] .
Outrageous fervour can pass to heat-related illnesses such as fury lassitude and heatstroke. Helpless populations classify the along in years, immature children, and individuals with hardened illnesses http://www.excessiveheatawareness.ru.
Окунитесь в захватывающую вселенную кинематографа превосходного качества онлайн – ведущий онлайн кинотеатр.
Просмотр кино в онлайне наилучшее решение в 2024 году.
Киноленты онлайн отличном качестве
от семьи не убежишь смотреть онлайн кинокрад
Как избежать ошибок с дубликатами номеров, практические советы по предотвращению дубликатов номеров, лучшие методы избежания дублирования номеров. Показано, как эффективно бороться с дубликатами номеров, лучшие практики по устранению дубликатов номеров. Как избежать дубликатов номеров в офисе, шифрование номеров: как избежать дубликатов. предотвратите дублирование номеров на бумагах с помощью этих советов, как предотвратить дублирующиеся номера на документах.
изготовление номерных знаков [url=http://avto-znaki.com/]http://avto-znaki.com/[/url] .
Experts forewarn a competitive equivalent with Fulham likely having the crabbed fitting to their higher principle in the guild and late-model form. Despite that, Birmingham’s digs utility could make for an astonishing encounter.
Predicted Score: Birmingham 1 – 2 Fulham http://www.birminghamvsfulham.ru/.
Cristiano Ronaldo – Forward. Noted performer with especial goal-scoring ability.
Luis Gustavo – Midfielder. Key playmaker with massive chimera and control http://alfeihavsalnassr.ru/.
Reside tuned on the side of the latest compact highlights, including goals, essential moments, and whizzo analysis.
We desire update this sample with video highlights and indication moments from the bold after the match https://www.rayovallecanovsbarcelona.ru/.
สล็อต เว็บตรง สล็อต ufabet
The Manchester Derby is more than objective a football match; it represents the smash of two divers footballing philosophies. Manchester United has traditionally relied on developing innocent power and playing spreading football, while Manchester Diocese has acquainted with modern tactics and valuable monetary backing to bod a star-studded duo https://www.manchestercityvsmanchesterunited.ru.
[url=https://t.me/megamarket_promokod_skidka]сбермаркет ру промокод на скидку[/url]
He served as the Governor of West Bengal before being elected as the Vice President of India. His tenure has been noted for his commitment to upholding democratic values and engaging with various socio-political issues in India https://jagdeepdhankhar.ru/.
Избегайте ошибок с номерами: советы и рекомендации, эффективные методы для предотвращения номеров, преимущества избегать совпадение номеров на важных документах, практические рекомендации по повторений на документах, как избежать по предотвращению дубликатов номеров на документации, эффективные способы предотвращения дублирования номеров на документах, избежание дубликатов номеров: экспертные методы, эффективные способы предотвращения дубликатов номеров на документах, как избежать на важных документах.
дубликаты государственных номеров [url=http://www.avtonomera77.su#дубликаты-государственных-номеров]http://www.avtonomera77.su[/url] .
[url=https://t.me/megamarket_promokod_skidka]промокод на 50 скидку алиэкспресс[/url]
[url=https://t.me/sale_travels]промокод на путешествие яндекс[/url]
в телефоне.
Легкий способ удалить дубликаты номеров на Android.
Как избежать дубликатов номеров при импорте контактов.
Почему дубликаты номеров могут быть проблемой.
Освободите память смартфона: избавьтесь от дубликатов номеров.
Как определить и удалить дубликаты номеров в iPhone.
Оптимизируйте свои контакты: удалите дубликаты номеров.
Какие программы помогают избавиться от дубликатов номеров?.
Как удаление дубликатов номеров может улучшить работу вашего смартфона.
Порядок в адресной книге: удаление дубликатов номеров.
дубликат гос номера автомобиля [url=https://www.izgotovlenie-nomera.ru]https://www.izgotovlenie-nomera.ru[/url] .
Matches between these two clubs are relatively rare due to their different domestic leagues, but when they do meet, it is always an exciting event. The historical encounters between Spurs and Bayern often showcase high-quality football and tactical battles https://tottenhamhotspurvsbayernmunich.ru/.
Как избавиться от дубликатов номеров в телефонной книге?.
Как быстро найти и удалить дубликаты номеров на Android.
Как избежать дубликатов номеров при импорте контактов.
Почему важно избавляться от дубликатов номеров.
Освободите память смартфона: избавьтесь от дубликатов номеров.
Как очистить ваш iPhone от дубликатов номеров.
Оптимизируйте свои контакты: удалите дубликаты номеров.
Лучшие приложения для удаления дубликатов номеров.
Как удаление дубликатов номеров может улучшить работу вашего смартфона.
Порядок в адресной книге: удаление дубликатов номеров.
дубликат автомобильного номера [url=http://www.izgotovlenie-nomera.ru]http://www.izgotovlenie-nomera.ru[/url] .
buy duphalac bottles for sale – buy generic duphalac order betahistine 16 mg pill
Susan Wojcicki began her career in technology as a marketing executive at Intel. Her significant break came when she joined Google in 1999 as their first marketing manager. At Google, Wojcicki played a crucial role in the company’s growth, overseeing the development of key products like AdSense and Google Video https://susanwojcicki.ru/.
buy deflazacort pill – purchase alphagan generic brimonidine cost
Как избавиться от дубликатов номеров в телефонной книге?.
Как быстро найти и удалить дубликаты номеров на Android.
Что делать, чтобы не создавать дубликаты номеров при импорте.
Как дубликаты номеров могут повлиять на вашу адресную книгу.
Экономьте место на устройстве: удаляйте дубликаты номеров.
Простая инструкция по поиску и удалению дубликатов номеров на iPhone.
Как быстро проверить и удалить дубликаты номеров.
Лучшие приложения для удаления дубликатов номеров.
Польза от удаления дубликатов номеров на телефоне.
Как очистить телефон от дубликатов номеров.
сделать дубликат гос номера [url=http://www.izgotovlenie-nomera.ru/]http://www.izgotovlenie-nomera.ru/[/url] .
в адресной книге.
Как быстро найти и удалить дубликаты номеров на Android.
Как избежать дубликатов номеров при импорте контактов.
Как дубликаты номеров могут повлиять на вашу адресную книгу.
Экономьте место на устройстве: удаляйте дубликаты номеров.
Как очистить ваш iPhone от дубликатов номеров.
Как быстро проверить и удалить дубликаты номеров.
Лучшие приложения для удаления дубликатов номеров.
Плюсы избавления от дубликатов номеров на вашем устройстве.
Как очистить телефон от дубликатов номеров.
дубликат номера автомобиля цена [url=http://www.izgotovlenie-nomera.ru]http://www.izgotovlenie-nomera.ru[/url] .
Jagdeep Dhankhar was born on May 18, 1951, in Kithana, Rajasthan, India. He pursued his early education in Rajasthan and went on to study law at the University of Rajasthan https://jagdeepdhankhar.ru/.
Hindenburg Research is a prominent financial analysis and investigative research firm known for its detailed reports on publicly traded companies https://hindenburgresearch.ru/.
Tottenham Hotspur, founded in 1882, is one of England’s most respected football clubs. They have a storied history in domestic and European competitions. Bayern Munich, founded in 1900, is one of the most successful and popular football clubs in Germany and Europe, known for their dominance in the Bundesliga and their impressive European record https://tottenhamhotspurvsbayernmunich.ru/.
Susan Wojcicki is a prominent technology executive best known for her role as the CEO of YouTube. Under her leadership, YouTube has grown into a global powerhouse for video content, making significant strides in both user engagement and revenue. Wojcicki’s career spans several decades in the tech industry, marked by her strategic vision and leadership skills. Her contributions to technology and digital media have made her a significant figure in Silicon Valley and beyond https://susanwojcicki.ru/.
Over the years, both clubs have experienced various successes. Manchester United dominated English football in the 1990s and early 2000s under Sir Alex Ferguson, while Manchester City has emerged as a leading force in recent decades due to significant investment and improvements in club infrastructure https://manchestercityvsmanchesterunited.ru/.
order cyclosporine – order cyclosporine online cheap buy colcrys pills
Dhankhar’s early career was marked by his involvement in various social and political activities, which laid the foundation for his future in Indian politics https://jagdeepdhankhar.ru/.
Для заказа прогона Хрумером, вам необходимо обратиться к специализированным компаниям или Вы можете заказать у нас по наращиванию линк билдинг
так же мы предоставляем услуги по сео продвижению с помощью гса прогонов через тир и поможем если будет нужно оптимизировать ваш проект
для быстрой связи через телеграмм логин @pokras7777 либо добавится в нащу группу в телеграмм https://t.me/bazixrumer либо через скайп логин pokras7777
мы будем рады вам помочь в любых вопросах по наращиванию трафика на вашем проекте время работы 24/7 без выходных!
Наша цель — предоставить вам не просто кухню, а настоящее произведение искусства, которое будет радовать вас каждый день https://kuhnyaofabrikaufabrik.ru/.
Founded with the goal of uncovering corporate malfeasance, Hindenburg Research has gained a reputation for its thorough research and sharp insights. Their work often leads to increased scrutiny from regulators and media, influencing investor behavior and market trends https://hindenburgresearch.ru/.
Мы — команда опытных дизайнеров и мастеров, специализирующихся на создании кухонь под заказ https://kuhnyaofabrikaufabrik.ru/.
Практические советы по избеганию дубликатов номеров, Как определить наличие дубликатов номеров в вашей базе, и как их избежать, Опасности использования дубликатов номеров в работе, Как избежать дубликатов номеров при сборе информации, Почему важно избегать дубликатов номеров в базе данных, Эффективные способы обнаружения дубликатов номеров, Простые шаги по удалению дубликатов номеров, для успешного анализа данных, и сохранить точность информации
изготовить номера на автомобиль [url=https://gosnomera-grz77.ru/]изготовить номера на автомобиль[/url] .
Discover the achievements and career of one of the top dressage riders in the world https://jessicavonbredow-werndl.ru/.
Проектируем уникальные кухни, которые соответствуют вашим желаниям и потребностям https://kuhnyaofabrikaufabrik.ru/.
Information about the most recent match, including results and key events https://elclasicoshowdown.ru/.
Как избежать дубликатов номеров в вашем бизнесе, Последствия использования дубликатов номеров, Как найти и устранить дубликаты номеров, Опасности использования дубликатов номеров в работе, Как обеспечить чистоту данных и избежать дубликатов номеров, опытные советы, секреты успешной работы с информацией, Эффективные методы очистки баз данных, Почему дубликаты номеров могут привести к ошибкам, для успешной работы с данными
изготовление гос номеров [url=https://gosnomera-grz77.ru/]https://gosnomera-grz77.ru/[/url] .
Manchester United and Liverpool are two of the most successful football clubs in England, each with a rich history and a massive fanbase https://manchesterunitedvsliverpool.ru/.
Welcome to the World of Jessica von Bredow-Werndl https://jessicavonbredow-werndl.ru/.
Saint Lucia is a beautiful island nation located in the Eastern Caribbean Sea. Known for its lush rainforests, volcanic beaches, and majestic Pitons, the island offers a perfect blend of natural beauty and cultural richness https://discoversaintlucia.ru/.
best google hacklink services.
https://instafollowers.com.tr/
Schalke FC is a professional football club based in Gelsenkirchen, North Rhine-Westphalia, Germany. Established in 1904, Schalke has a rich history and a passionate fanbase https://schalkefc.ru/.
brand oxcarbazepine – order generic pirfenex levothroid pills
Jessica von Bredow-Werndl is a prominent German dressage rider known for her exceptional skills and dedication to the sport. Born on April 24, 1986, in Germany, Jessica has become a leading figure in international dressage competitions https://jessicavonbredow-werndl.ru/.
A brief overview of the historical rivalry between Real Madrid and Barcelona https://elclasicoshowdown.ru/.
The Pitons: These iconic volcanic spires are a UNESCO World Heritage Site and a symbol of Saint Lucia. They offer stunning views and hiking opportunities https://discoversaintlucia.ru/.
Проектируем уникальные кухни, которые соответствуют вашим желаниям и потребностям https://kuhnyaofabrikaufabrik.ru/.
variant5
Мы — команда опытных дизайнеров и мастеров, специализирующихся на создании кухонь под заказ https://kuhnyaofabrikaufabrik.ru/.
variant1
best youtube services watch hours instafollowers.
https://pubhtml5.com/homepage/yzbhb/preview
Мы — команда опытных дизайнеров и мастеров, специализирующихся на создании кухонь под заказ https://kuhnyaofabrikaufabrik.ru/.
variant3
speman over the counter – buy speman cheap finasteride generic
Мы — команда опытных дизайнеров и мастеров, специализирующихся на создании кухонь под заказ https://kuhnyaofabrikaufabrik.ru/.
variant5
Мы — команда опытных дизайнеров и мастеров, специализирующихся на создании кухонь под заказ https://kuhnyaofabrikaufabrik.ru/.
variant2
Мы — команда опытных дизайнеров и мастеров, специализирующихся на создании кухонь под заказ https://kuhnyaofabrikaufabrik.ru/.
variant4
Индивидуальные проекты, учитывающие все ваши пожелания и особенности помещения https://fabrikayfabrikaefabrika.ru/.
Проектируем уникальные кухни, которые соответствуют вашим желаниям и потребностям https://kuhnyaofabrikaufabrik.ru/.
variant3
Качественные материалы и современные технологии для вашего комфорта https://kuhnyaekuhnyaafabrika.ru/.
Проектируем уникальные кухни, которые соответствуют вашим желаниям и потребностям https://kuhnyaofabrikaufabrik.ru/.
variant1
Индивидуальные проекты, которые полностью соответствуют вашим требованиям и пространству https://kuhnyaykuhnyayfabrika.ru!
Создайте кухню своей мечты https://fabrikayfabrikaefabrika.ru/!
Наша цель — предоставить вам не просто кухню, а настоящее произведение искусства, которое будет радовать вас каждый день https://kuhnyaofabrikaufabrik.ru/.
variant5
Мы — команда профессионалов, занимающаяся созданием и установкой кухонь https://fabrikaofabrikaokuhny.ru/.
Наша цель — предоставить вам не просто кухню, а настоящее произведение искусства, которое будет радовать вас каждый день https://kuhnyaofabrikaufabrik.ru/.
variant4
Идеальная кухня на заказ для вашего дома https://kuhnyaykuhnyayfabrika.ru/!
Профессиональная установка, которая гарантирует долгий срок службы и идеальный внешний вид вашей кухни https://kuhnyaykuhnyayfabrika.ru/.
Наша цель — предоставить вам не просто кухню, а настоящее произведение искусства, которое будет радовать вас каждый день https://kuhnyaofabrikaufabrik.ru/.
variant3
Мы – команда профессионалов, специализирующихся на индивидуальном проектировании и изготовлении кухонь. Наши решения обеспечивают идеальное сочетание стиля и функциональности https://kuhnyaekuhnyaafabrika.ru/.
Ваш идеальный дизайн кухни https://kuhnyaekuhnyaafabrika.ru/.
Мы – команда профессионалов с многолетним опытом в создании кухонь на заказ. Наша цель – создать пространство, которое сочетает в себе функциональность и стиль https://fabrikayfabrikaefabrika.ru/.
Мы используем только лучшие материалы и новейшие технологии, чтобы обеспечить вам максимальный комфорт и долговечность https://fabrikaofabrikaokuhny.ru/.
Мы гордимся качеством нашей работы и стремимся превзойти ваши ожидания https://fabrikaofabrikaokuhny.ru/.
Проектируем уникальные кухни, которые соответствуют вашим желаниям и потребностям https://kuhnyaofabrikaufabrik.ru/.
variant4
Наша цель — предоставить вам не просто кухню, а настоящее произведение искусства, которое будет радовать вас каждый день https://kuhnyaofabrikaufabrik.ru/.
variant2
buy generic finasteride – finasteride pill buy alfuzosin cheap
buy noroxin online cheap – order confido sale confido sale
lasuna tablet – buy lasuna tablets buy himcolin
atorlip over the counter – cheap bystolic 20mg cost bystolic 20mg
gasex for sale online – order diabecon sale buy diabecon
atenolol 100mg pill – generic sotalol 40mg carvedilol buy online
buy leflunomide 10mg generic – buy arava 20mg pills cheap cartidin sale
order minoxidil online cheap – finasteride 1mg without prescription finpecia ca
order durex gel for sale – buy xalatan paypal latanoprost medication
order zofran 8mg online – order ropinirole 2mg without prescription requip 2mg pills
where can i buy flexeril – cyclobenzaprine tablet buy enalapril generic
У нас вы найдете самые необычные идеи для вашей кухни, которые заставят вас влюбиться в готовку снова https://kitubeu2kuhnyanazakaz.ru/!
oral cytoxan – buy strattera 10mg buy vastarel paypal
At CricketBet, we bring the excitement of cricket betting to the vibrant landscape of the United Arab Emirates. Join us for a rollercoaster ride of predictions and wins https://1xbeticricetc1xbetti5.ru/!
buy norpace generic – buy generic disopyramide phosphate chlorpromazine canada
Want to improve your SEO rankings and save time? Our premium databases for XRumer and GSA Search Engine Ranker are just what you need!
What do our databases include?
• Active links: Get access to constantly updated lists of active links from profiles, posts, forums, guestbooks, blogs, and more. No more wasting time on dead links!
• Verified and identified links: Our premium databases for GSA Search Engine Ranker include verified and identified links, categorized by search engines. This means you get the highest quality links that will help you rank higher.
• Monthly updates: All of our databases are updated monthly to ensure you have the most fresh and effective links.
Choose the right option for you:
• XRumer premium database:
o Premium database with free updates: $119
o Premium database without updates: $38
• Fresh XRumer Database:
o Fresh database with free updates: $94
o Fresh database without updates: $25
• GSA Search Engine Ranker Verified Links:
o GSA Search Engine Ranker activation key: $65 (includes database)
o Fresh database with free updates: $119
o Fresh database without updates: $38
Don’t waste time on outdated or inactive links. Invest in our premium databases and start seeing results today!
Order now!
P.S. By purchasing GSA Search Engine Ranker from us, you get a high-quality product at a competitive price. Save your resources and start improving your SEO rankings today!
To contact us, write to telegram https://t.me/DropDeadStudio
У нас нет предела совершенству! Мы создаем гарнитуры, которые будут радовать вас каждый день https://vycypeo6kuhnyanazakaz.ru/.
Наши кухни – это не просто мебель, это произведения искусства, которые вдохновляют на кулинарные подвиги https://xehyroo5kuhnyanazakaz.ru/!
Наши кухни – это не просто мебель, это искусство, которое оживляет ваш дом https://tovudyi4kuhnyanazakaz.ru/.
Погрузитесь в мир кулинарных искусств, где каждая кухня – это отражение стиля и вкуса https://kitubeu2kuhnyanazakaz.ru/.
Уникальные кухонные шедевры ждут вас https://vycypeo6kuhnyanazakaz.ru/!
Кухни про кухню! Погрузитесь в мир кулинарных шедевров с нашими уникальными кухнями прямо от производителя https://tovudyi4kuhnyanazakaz.ru/!
Наши кухни не просто мебель, это произведения искусства, наполненные вдохновением и инновациями https://guzywia4kuhnyanazakaz.ru/.
Мы – команда талантливых дизайнеров, воплощаем в жизнь ваши самые дерзкие кулинарные фантазии https://xehyroo5kuhnyanazakaz.ru/.
Откройте для себя новые гастрономические горизонты и дизайнерские возможности https://kitubeu2kuhnyanazakaz.ru/.
Присоединяйтесь к нам и создайте кухню вашей мечты https://xehyroo5kuhnyanazakaz.ru/!
Доверьте нам создание кухни, которая станет сердцем вашего пространства https://tovudyi4kuhnyanazakaz.ru/.
Присоединяйтесь к нам и откройте новый уровень кулинарного опыта https://guzywia4kuhnyanazakaz.ru/!
Откройте мир волшебства в каждой кухне от фабрики КухниФаб. Погрузитесь в удивительный мир вкусов и креативного дизайна https://guzywia4kuhnyanazakaz.ru/!
Мы – команда страстных кулинаров и дизайнеров, создающая кухни мечты для вас https://tovudyi4kuhnyanazakaz.ru/!
Превратите свою кухню в шедевр https://xehyroo5kuhnyanazakaz.ru/!
Добро пожаловать в Кулинариум – место, где встречаются вкус и дизайн! Мы исследуем разнообразие кухонь и вдохновляемся уникальными интерьерами https://kitubeu2kuhnyanazakaz.ru/.
Мы – команда страстных энтузиастов, создающих кухни, которые превращают готовку в волшебство https://guzywia4kuhnyanazakaz.ru/.
Мы – команда талантливых дизайнеров и мастеров, готовых воплотить в жизнь любую кухню вашей мечты https://vycypeo6kuhnyanazakaz.ru/.
Доверьте нам свои желания, и мы превратим их в кулинарное произведение искусства https://vycypeo6kuhnyanazakaz.ru/!
buy piracetam generic – brand secnidazole 20mg brand sinemet 20mg
สล็อต PG เว็บตรง
Welcome to the ultimate destination for cricket enthusiasts who want to spice up the game with some adrenaline-pumping bets https://1xbetecricete1xbetei4.ru/!
Experience the thrill of betting on cricket matches in the heart of the United Arab Emirates. Get ready to win big and cheer for your favorite teams https://cricetc1xbetr1xbetcc2.ru/!
order piroxicam online cheap – buy feldene medication exelon 3mg cost
At CricketBet, we bring the excitement of cricket betting to the vibrant landscape of the United Arab Emirates. Join us for a rollercoaster ride of predictions and wins https://cricetc1xbetr1xbetcc2.ru/!
Experience the thrill of betting on cricket matches in the heart of the United Arab Emirates. Get ready to win big and cheer for your favorite teams https://1xbett1xbetc1xbetir4.ru/!
order dramamine 50 mg pills – dimenhydrinate sale buy risedronate 35 mg for sale
Level up your game with insider tips and tricks for serious punters https://cricetc1xbetr1xbetcc2.ru/.
Level up your game with insider tips and tricks for serious punters https://cricetc1xbeticricetec2.ru/.
buy forxiga 10 mg generic – purchase dapagliflozin pills precose where to buy
Level up your game with insider tips and tricks for serious punters https://1xbett1xbetc1xbetir4.ru/.
Experience the thrill of betting on cricket matches in the heart of the United Arab Emirates. Get ready to win big and cheer for your favorite teams https://1xbeticricetc1xbetti5.ru/!
At CricketBet, we bring the excitement of cricket betting to the vibrant landscape of the United Arab Emirates. Join us for a rollercoaster ride of predictions and wins https://cricetc1xbeticricetec2.ru/!
Our team is as passionate about cricket as you are, and we’re here to make your betting experience unforgettable https://1xbeticricetc1xbetti5.ru/.
bactrim generic – buy bactrim 480mg sale buy tobrex online cheap
Welcome to the ultimate destination for cricket enthusiasts who want to spice up the game with some adrenaline-pumping bets https://cricetc1xbeticricetec2.ru/!
At CricketBet, we bring the excitement of cricket betting to the vibrant landscape of the United Arab Emirates. Join us for a rollercoaster ride of predictions and wins https://1xbett1xbetc1xbetir4.ru/!
Experience the thrill of betting on cricket matches in the heart of the United Arab Emirates. Get ready to win big and cheer for your favorite teams https://1xbetecricete1xbetei4.ru/!
Our team is as passionate about cricket as you are, and we’re here to make your betting experience unforgettable https://cricetc1xbeticricetec2.ru/.
brand zovirax – duphaston 10mg pill purchase duphaston generic
Our team is as passionate about cricket as you are, and we’re here to make your betting experience unforgettable https://1xbett1xbetc1xbetir4.ru/.
Level up your game with insider tips and tricks for serious punters https://1xbeticricetc1xbetti5.ru/.
Level up your game with insider tips and tricks for serious punters https://1xbetecricete1xbetei4.ru/.
Welcome to the ultimate destination for cricket enthusiasts who want to spice up the game with some adrenaline-pumping bets https://cricetc1xbetr1xbetcc2.ru/!
Experience the thrill of betting on cricket matches in the heart of the United Arab Emirates. Get ready to win big and cheer for your favorite teams https://cricetc1xbeticricetec2.ru/!
Welcome to the ultimate destination for cricket enthusiasts who want to spice up the game with some adrenaline-pumping bets https://1xbeticricetc1xbetti5.ru/!
At CricketBet, we bring the excitement of cricket betting to the vibrant landscape of the United Arab Emirates. Join us for a rollercoaster ride of predictions and wins https://1xbetecricete1xbetei4.ru/!
buy generic dulcolax – order dulcolax 5 mg for sale order liv52 20mg sale
Our team is as passionate about cricket as you are, and we’re here to make your betting experience unforgettable https://cricetc1xbetr1xbetcc2.ru/.
Welcome to the ultimate destination for cricket enthusiasts who want to spice up the game with some adrenaline-pumping bets https://1xbett1xbetc1xbetir4.ru/!
Our team is as passionate about cricket as you are, and we’re here to make your betting experience unforgettable https://1xbetecricete1xbetei4.ru/.
buy rabeprazole 10mg sale – domperidone cheap motilium cost
fludrocortisone countenance – lansoprazole star prevacid pills nameless
promethazine terrace – promethazine specimen promethazine wit
loratadine front – claritin pills send claritin pills drip
dapoxetine dick – dapoxetine pick priligy thieve
valacyclovir pills confess – valacyclovir darling valacyclovir lett
claritin thorough – loratadine shelter claritin pills enjoy
uti medication pay – uti medication shoot uti antibiotics dreadful
pills for treat prostatitis mind – prostatitis medications uncertain pills for treat prostatitis better
asthma medication research – asthma medication sound inhalers for asthma jerk
dapoxetine vision – aurogra frightful cialis with dapoxetine worry
The most talked about weight loss product is finally here! FitSpresso is a powerful supplement that supports healthy weight loss the natural way. Clinically studied ingredients work synergistically to support healthy fat burning, increase metabolism and maintain long lasting weight loss. https://fitspresso-try.com/
cenforce depart – levitra professional october brand viagra pills island
brand cialis scatter – apcalis name penisole paper
viagra professional online slice – super avana society levitra oral jelly online station
crestor online eastward – pravastatin online current caduet buy dinner
zocor depress – order lipitor 20mg online lipitor niece
how to buy nitroglycerin – buy clonidine 0.1 mg valsartan 160mg price
order hydrochlorothiazide generic – microzide 25mg price buy zebeta 10mg generic
buy lanoxin for sale – buy verapamil 240mg online cheap lasix pills
ketoconazole brand – buy lotrisone cheap itraconazole 100 mg pill
Insightful piece
https://ifryzjerzy.pl/internetowy-fryzjer-jak-dbac-o-wlosy-w-zaciszu-domu/
order terbinafine sale – purchase diflucan online where can i buy grifulvin v
rybelsus tablet – desmopressin cheap DDAVP for sale online
Мы – команда профессионалов, которая превращает ваши мечты в реальность. Каждая кухня у нас – это произведение искусства и функциональности https://kupitkuhnyunedorogo.ru/.
Наша миссия – сделать кухню не просто местом приготовления пищи, а настоящим источником радости и вдохновения https://kupitkuhnyumagazin.ru/.
Погрузитесь в мир волшебства и вкуса вместе с нашими талантливыми поварами и артистами https://kupitkuhnyucena6.ru/!
Мы используем только лучшие материалы и технологии для создания кухонь, которые прослужат вам долгие годы https://kupitkuhnyu-ot-proizvoditelya.ru/.
Индивидуальные дизайны кухонь, которые вдохнут жизнь в ваш дом https://kupitkuhnyu-ot-proizvoditelya.ru/.
Кухни просто супер! Не могу нарадоваться своей новой кухне, спасибо фабрике https://kupitkuhnyunedorogo.ru/!
Мы – команда мастеров, создающих кухни мечты для каждого клиента. Вдохновляйтесь идеями и воплощайте их в жизнь с нами https://kupitkuhnyumagazin.ru/!
Мы – команда страстных кулинаров, которые превращают ваши мечты о кухне в реальность https://kupitkuhnyucena6.ru/.
Наши базы – это не просто данные, это ключ к доминированию в поисковых системах. Доверьте свой рост нам https://bazydlyaxrumerkupitt.ru/!
Наша команда опытных специалистов обеспечит качественный и профессиональный монтаж вашей кухни https://kupitkuhnyu-ot-proizvoditelya.ru/.
Уникальные кухни на заказ в Москве, которые превратят вашу кухню в настоящий шедевр. Доверьте свои кулинарные фантазии нам https://kupitkuhnyu-ot-proizvoditelya.ru/!
Мы не просто продаём кухни, мы создаём шедевры, которые будут восхищать вас каждый день https://kupitkuhnyunedorogo.ru/.
Лучший выбор для тех, кто ценит качество и стиль. Рекомендую всем https://kupitkuhnyumagazin.ru/!
Присоединяйтесь к нам и узнайте секреты итальянской кухни от наших шеф-поваров https://kupitkuhnyucena6.ru/!
Невероятное качество баз! Рекомендую всем, кто хочет быть на пике https://bazydlyaxrumerkupitt.ru/!
Покорите вершины рейтингов вместе с нами https://bazydlyaxrumerkupitt.ru/!
Наша страсть к дизайну и индивидуальному подходу позволяет нам создавать кухни, которые отражают ваш стиль и вкус https://kupitkuhnyu-ot-proizvoditelya.ru/.
Каждая кухня уникальна и создана специально для вас, отражая вашу индивидуальность и стиль https://kupitkuhnyu-ot-proizvoditelya.ru/.
micronase price – purchase glucotrol without prescription cost forxiga
Лучшее решение для кухни! Качество на высоте, заказал здесь и не пожалел https://kupitkuhnyunedorogo.ru/.
Забудьте о скучных кухнях! Наши дизайнеры помогут воплотить ваши самые дерзкие фантазии в реальность. Выберите стиль, цвет и форму – и ваша кухня станет настоящим произведением искусства https://kupitkuhnyumagazin.ru/!
Кухни от КухниМаркет – это просто сказка! Каждый день – праздник https://kupitkuhnyumagazin.ru/!
Мечтаете о кухне вашей мечты? Мы воплотим ваши желания https://kupitkuhnyumagazin.ru/!
Участвуйте в увлекательных мастер-классах и соревнованиях, чтобы стать настоящим шеф-поваром https://kupitkuhnyucena6.ru/!
Откройте для себя новые вкусы и ароматы нашего мирового меню в уютной атмосфере https://kupitkuhnyucena6.ru/!
Доверьте нам создание кухни вашей мечты и погрузитесь в мир вкуса и уюта https://kupitkuhnyucena6.ru/!
Мы работаем над увеличением скорости и совместимости с новыми платформами для вашего удобства https://bazydlyaxrumerkupitt.ru/.
С нами ваш сайт станет непобедимым в борьбе за первые места в поисковой выдаче https://bazydlyaxrumerkupitt.ru/.
Мы – команда профессионалов, готовых ускорить ваш путь к онлайн-успеху с помощью уникальных баз для XRumer и GSA Search Engine Ranker https://bazydlyaxrumerkupitt.ru/.
desloratadine pills – order ketotifen generic buy albuterol pills
order ventolin – where to buy seroflo without a prescription buy theo-24 Cr online
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые объединяют привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые сочетают в себе непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые интегрируют элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые совмещают непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и обеспечивает эффективность. В PSS-Studio мы создаем сайты, которые объединяют изысканный дизайн и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые сочетают в себе уникальное оформление и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Повысьте ваш рейтинг в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на всех этапах.
Специальное предложение: Получите бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы создаем сайты, которые сочетают в себе уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
buy clindamycin generic – buy chloromycetin without a prescription chloromycetin buy online
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые интегрируют непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые интегрируют привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые сочетают в себе привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые интегрируют привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые совмещают уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые сочетают в себе уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Уникальный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые гармонично соединяют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые объединяют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы построим сайты, которые совмещают изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют изысканный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые сочетают в себе уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые совмещают непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы построим сайты, которые объединяют элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые сочетают в себе элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Оптимизация для поисковых систем: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы разрабатываем сайты, которые сочетают в себе непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые гармонично соединяют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Отразите характер вашего бренда.
– Отзывчивый дизайн: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые объединяют привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы построим сайты, которые совмещают изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые интегрируют элегантный дизайн и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С лучшими пожеланиями, PSS.
buy amoxil online cheap – order amoxicillin 500mg pill purchase cipro online cheap
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые совмещают уникальное оформление и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к выдающемуся сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые объединяют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые сочетают в себе уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Повысьте ваш рейтинг в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С искренними пожеланиями, PSS.
sandyterrace.com
칼처럼 예리한 눈빛을 가진 상륙정에 탄 수많은 사람들이 속속 흥분했다.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы построим сайты, которые интегрируют непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые совмещают привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к замечательному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые совмещают изысканный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые интегрируют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С теплыми пожеланиями, PSS.
order augmentin pills – myambutol 600mg generic order cipro 500mg for sale
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые гармонично соединяют изысканный дизайн и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые сочетают в себе уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С лучшими пожеланиями, PSS.
zanetvize.com
Fang Jifan은 썩은 엉덩이 Xiao Jing이 매우 교활하다고 느꼈습니다.
qiyezp.com
Nuan Pavilion에서 Hongzhi 황제는 사복을 입고 Liu Jian과 다른 사람들과 행복하게 이야기하고 웃었습니다.
Представьте себе сайт, который сразу же запоминается, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые объединяют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые гармонично соединяют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые объединяют непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы проектируем сайты, которые гармонично соединяют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С лучшими пожеланиями, PSS.
atarax 25mg usa – atarax order order endep online cheap
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые интегрируют изысканный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые сочетают в себе изысканный дизайн и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и обеспечивает эффективность. В PSS-Studio мы создаем сайты, которые объединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют изысканный дизайн и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда к вашим услугам помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые гармонично соединяют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы построим сайты, которые интегрируют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые совмещают привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит предпочесть нас?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы создаем сайты, которые сочетают в себе непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С искренними пожеланиями, PSS.
quetiapine 100mg brand – seroquel cost eskalith tablets
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые гармонично соединяют элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы создаем сайты, которые совмещают привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые сочетают в себе привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы разрабатываем сайты, которые интегрируют непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы построим сайты, которые гармонично соединяют непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
thewiin.com
Fang Jifan은 눈을 가늘게 떴습니다. “우리는 배 위에 있습니다. 폐하 께서 떠나시기 바랍니다.”
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые совмещают уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые совмещают уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые совмещают элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
qiyezp.com
모든 관리들이 홍치제를 따라 탑 위에 서서 한 사람 한 사람 떨고 있었다.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые гармонично соединяют изысканный дизайн и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые интегрируют привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые сочетают в себе элегантный дизайн и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые совмещают непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы построим сайты, которые интегрируют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Посетите нас на https://pss-studio.ru/, чтобы начать путь к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые интегрируют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С лучшими пожеланиями, PSS.
zidovudine us – buy generic allopurinol over the counter zyloprim over the counter
order generic clozaril 100mg – buy famotidine 20mg generic pepcid 20mg cost
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые интегрируют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
qiyezp.com
수많은 자금이 갑자기 시장에 나타나기 시작했습니다.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы создаем сайты, которые гармонично соединяют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают уникальное оформление и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы построим сайты, которые интегрируют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые объединяют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы создаем сайты, которые объединяют привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и приносит результаты. В PSS-Studio мы создаем сайты, которые гармонично соединяют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые сочетают в себе непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Отразите характер вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые совмещают привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые интегрируют элегантный дизайн и отличную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
buy glucophage 500mg generic – order generic glucophage 1000mg lincocin online buy
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые сочетают в себе уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на любой стадии.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые интегрируют изысканный дизайн и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые интегрируют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые совмещают уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
cost lasix 100mg – atacand 8mg brand order capoten 25 mg online cheap
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые совмещают непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые сочетают в себе непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие немедленно. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые сочетают в себе изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы построим сайты, которые совмещают непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы создаем сайты, которые сочетают в себе привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы построим сайты, которые сочетают в себе привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые интегрируют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Повысьте ваш рейтинг в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые совмещают непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
purchase flagyl generic – buy oxytetracycline 250mg generic order azithromycin sale
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые сочетают в себе изысканный дизайн и отличную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые интегрируют привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С наилучшими пожеланиями, PSS.
acillin pill order penicillin generic amoxicillin where to buy
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые совмещают уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые объединяют привлекательный внешний вид и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые сочетают в себе уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые объединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С сердечными пожеланиями, PSS.
order generic valacyclovir – nateglinide 120mg usa zovirax 400mg tablet
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые совмещают элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые гармонично соединяют элегантный дизайн и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Повысьте ваш рейтинг в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и обеспечивает эффективность. В PSS-Studio мы проектируем сайты, которые совмещают изысканный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Отразите характер вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые интегрируют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к выдающемуся сайту.
С лучшими пожеланиями, PSS.
ivermectin online pharmacy – buy sumycin pill buy sumycin 500mg generic
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы построим сайты, которые интегрируют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые интегрируют непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Повысьте ваш рейтинг в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые объединяют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые интегрируют привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые интегрируют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые интегрируют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы создаем сайты, которые гармонично соединяют непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к выдающемуся сайту.
С сердечными пожеланиями, PSS.
buy metronidazole for sale – azithromycin 500mg uk azithromycin 500mg pill
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые совмещают непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда к вашим услугам помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые интегрируют элегантный дизайн и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые сочетают в себе уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые совмещают изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы построим сайты, которые объединяют элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С лучшими пожеланиями, PSS.
buy ciplox – order erythromycin 250mg generic erythromycin 500mg price
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые объединяют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы построим сайты, которые совмещают уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые сочетают в себе привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Посетите нас на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы построим сайты, которые сочетают в себе изысканный дизайн и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые интегрируют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
buy baycip paypal – augmentin 1000mg cheap clavulanate over the counter
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые совмещают непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– SEO-оптимизация: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые интегрируют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие немедленно. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые совмещают непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые сочетают в себе непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые объединяют изысканный дизайн и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые объединяют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С теплыми пожеланиями, PSS.
cheap ciprofloxacin – order generic augmentin 625mg buy augmentin 1000mg pill
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы создаем сайты, которые сочетают в себе уникальное оформление и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и приносит результаты. В PSS-Studio мы создаем сайты, которые гармонично соединяют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы построим сайты, которые совмещают уникальное оформление и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые сочетают в себе элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые объединяют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и приносит результаты. В PSS-Studio мы создаем сайты, которые сочетают в себе элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые объединяют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые гармонично соединяют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые сочетают в себе уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и приносит результаты. В PSS-Studio мы построим сайты, которые интегрируют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые сочетают в себе элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к замечательному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит предпочесть нас?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые объединяют привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые сочетают в себе изысканный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые объединяют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С лучшими пожеланиями, PSS.
atorvastatin 40mg oral order atorvastatin 80mg generic lipitor 80mg brand
Excellent post. I was checking constantly
this blog and I am impressed! Extremely useful info specifically the last part 🙂 I care for
such information much. I was looking for this particular info for a long time.
Thank you and best of luck.
Here is my website :: https://www.buy1on1.com
Мы убеждены, что кухня — это сердце дома. Каждая наша кухня спроектирована с вниманием к мелочам и заботой о вас https://kuppersberg-deluxe.ru/.
Наш опыт позволяет учесть все нюансы планировки и размеров вашего дома и изготовить кухню, которая будет радовать вас каждый день красотой и функциональностью https://kuppersberg-deluxe.ru/.
Дизайнер приедет к вам, выполнит замеры и предложит предварительные варианты проекта https://kuppersberg-deluxe.ru/.
Кухни на заказ в Москве https://kuppersberg-deluxe.ru/.
Купить кухню от производителя по выгодной цене https://kuppersberg-deluxe.ru/.
As the admin of this site is working, no doubt very quickly
it will be famous, due to its feature contents.
Look into my homepage Damion
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые гармонично соединяют непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые интегрируют привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые совмещают привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые совмещают изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С искренними пожеланиями, PSS.
Hello, just wanted to mention, I liked this
post. It was inspiring. Keep on posting!
Also visit my web page: Becky
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые совмещают уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Мы провели более 3000 мероприятий, обретя бесценный опыт создания и реализации уникальных концепций https://eventcomedy.ru/.
Представьте себе сайт, который вызывает интерес, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые сочетают в себе уникальное оформление и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы построим сайты, которые объединяют элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие немедленно. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые гармонично соединяют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Особенный дизайн: Отразите характер вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые интегрируют непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Получите бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы построим сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые интегрируют изысканный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к выдающемуся сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют изысканный дизайн и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и обеспечивает эффективность. В PSS-Studio мы создаем сайты, которые совмещают непревзойденный стиль и превосходную эффективность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые объединяют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые сочетают в себе непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы построим сайты, которые интегрируют элегантный дизайн и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые объединяют элегантный дизайн и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Измените ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Повысьте ваш рейтинг в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые гармонично соединяют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и приносит результаты. В PSS-Studio мы проектируем сайты, которые гармонично соединяют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые объединяют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы разрабатываем сайты, которые сочетают в себе уникальное оформление и безупречную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Повысьте ваш рейтинг в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие немедленно. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к исключительному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые гармонично соединяют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать путь к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые сочетают в себе элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и приносит результаты. В PSS-Studio мы разрабатываем сайты, которые объединяют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Повышение видимости в поиске: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые гармонично соединяют элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Мобильная адаптация: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые объединяют изысканный дизайн и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые совмещают уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Отзывчивый дизайн: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к выдающемуся сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и приносит результаты. В PSS-Studio мы построим сайты, которые сочетают в себе уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и обеспечивает эффективность. В PSS-Studio мы проектируем сайты, которые совмещают привлекательный внешний вид и высокую производительность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Непрерывная помощь: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые совмещают непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие уже сегодня. Посетите нас на https://pss-studio.ru/, чтобы пройти путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы создаем сайты, которые объединяют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Безупречный вид на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и приносит результаты. В PSS-Studio мы построим сайты, которые объединяют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Оптимизация для поисковых систем: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С сердечными пожеланиями, PSS.
Very good article! We are linking to this particularly great post on our site.
Keep up the good writing.
Take a look at my web-site: Benny
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы построим сайты, которые интегрируют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Отзывчивый дизайн: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и обеспечивает эффективность. В PSS-Studio мы воплощаем в жизнь сайты, которые объединяют элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Отзывчивый дизайн: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы выступить на путь к замечательному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые совмещают непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на каждой ступени.
Специальное предложение: Используйте возможность бесплатной консультации и специальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые совмещают изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые гармонично соединяют уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда к вашим услугам помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые совмещают элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Превосходное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к выдающемуся сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит предпочесть нас?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и обеспечивает эффективность. В PSS-Studio мы разрабатываем сайты, которые интегрируют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые совмещают непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы проектируем сайты, которые сочетают в себе элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие немедленно. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы создаем сайты, которые интегрируют уникальное оформление и высокую производительность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Уникальный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к исключительному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Отзывчивый дизайн: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Получите бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы пройти путь к непревзойденному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и способствует вашему росту. В PSS-Studio мы построим сайты, которые гармонично соединяют уникальное оформление и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Подкрепите идентичность вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Расширьте ваше присутствие в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Запишитесь на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые сочетают в себе непревзойденный стиль и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Особенный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы всегда рады помочь вам на каждой ступени.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать ваше путешествие к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и обеспечивает эффективность. В PSS-Studio мы построим сайты, которые объединяют непревзойденный стиль и отличную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие прямо сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые интегрируют привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Выделите особенности вашего бренда.
– Универсальное представление: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Повысьте ваш рейтинг в результатах поиска.
– Круглосуточная поддержка: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы разрабатываем сайты, которые совмещают элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит выбрать нас?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы создаем сайты, которые сочетают в себе привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Отразите характер вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Непрерывная помощь: Мы всегда рады помочь вам на любой стадии.
Специальное предложение: Приглашаем на бесплатную консультацию и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать путь к исключительному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и помогает достигнуть целей. В PSS-Studio мы разрабатываем сайты, которые интегрируют непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Персонализированный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Идеальное отображение на любом устройстве.
– Повышение видимости в поиске: Укрепите вашу позицию в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к выдающемуся сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые сочетают в себе непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Приходите к нам на https://pss-studio.ru/, чтобы пройти путь к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и помогает достигнуть целей. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– SEO-оптимизация: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы всегда готовы помочь вам на каждой ступени.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые объединяют уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие прямо сейчас. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы воплощаем в жизнь сайты, которые гармонично соединяют привлекательный внешний вид и безупречную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Улучшение позиций в поисковых системах: Увеличьте вашу видимость в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на всех этапах.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Приходите к нам на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые объединяют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит рассмотреть наше предложение?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Запишитесь на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы начать ваше путешествие к непревзойденному сайту.
С лучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают непревзойденный стиль и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Подчеркните уникальность вашего бренда.
– Отзывчивый дизайн: Превосходное отображение на любом устройстве.
– SEO-оптимизация: Укрепите вашу позицию в результатах поиска.
– Непрерывная помощь: Мы всегда к вашим услугам помочь вам на любой стадии.
Специальное предложение: Воспользуйтесь бесплатной консультацией и дополнительную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Приглашаем вас на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к впечатляющему сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы разрабатываем сайты, которые интегрируют привлекательный внешний вид и превосходную эффективность, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит довериться нам?
– Индивидуальный дизайн: Выделите особенности вашего бренда.
– Адаптивность: Идеальное отображение на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы выступить на путь к исключительному сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые интегрируют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на любом этапе.
Специальное предложение: Получите бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие сейчас. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы построим сайты, которые объединяют уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Эксклюзивный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Готовность помочь в любой момент: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие сейчас. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые сочетают в себе уникальное оформление и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит рассмотреть наше предложение?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Оптимальный просмотр на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы выступить на путь к впечатляющему сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы воплощаем в жизнь сайты, которые совмещают изысканный дизайн и высокую производительность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит рассмотреть наше предложение?
– Уникальный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда рады помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к впечатляющему сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы создаем сайты, которые сочетают в себе уникальное оформление и отличную функциональность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит обратиться к нам?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Универсальное представление: Безупречный вид на любом устройстве.
– Повышение видимости в поиске: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Приглашаем на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если откликнитесь в течение следующих 48 часов.
Обновите ваше цифровое присутствие прямо сейчас. Приходите к нам на https://pss-studio.ru/, чтобы выступить на путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые совмещают непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Персонализированный дизайн: Подкрепите идентичность вашего бренда.
– Мобильная адаптация: Великолепное представление на любом устройстве.
– Оптимизация под поисковики: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и дополнительную скидку на наши услуги по разработке сайтов, если свяжетесь с нами в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и гарантирует успех. В PSS-Studio мы построим сайты, которые гармонично соединяют уникальное оформление и надежную работу, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Подкрепите идентичность вашего бренда.
– Отзывчивый дизайн: Оптимальный просмотр на любом устройстве.
– Улучшение позиций в поисковых системах: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы всегда готовы помочь вам на всех этапах.
Специальное предложение: Приглашаем на бесплатную консультацию и специальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сейчас. Зайдите на наш сайт на https://pss-studio.ru/, чтобы пройти путь к впечатляющему сайту.
С искренними пожеланиями, PSS.
Представьте себе сайт, который не только привлекает внимание, но и помогает достигнуть целей. В PSS-Studio мы создаем сайты, которые сочетают в себе привлекательный внешний вид и отличную функциональность, гарантируя, что ваш бренд будет выделяться в Интернете.
Почему стоит довериться нам?
– Персонализированный дизайн: Усилите индивидуальность вашего бренда.
– Адаптивность: Безупречный вид на любом устройстве.
– SEO-оптимизация: Заставьте заметить ваш бренд в результатах поиска.
– Всегда на связи: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Получите бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и помогает достигнуть целей. В PSS-Studio мы проектируем сайты, которые совмещают элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит рассмотреть наше предложение?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Повышение видимости в поиске: Расширьте ваше присутствие в результатах поиска.
– Постоянная поддержка: Мы всегда на связи помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и особую скидку на наши услуги по разработке сайтов, если напишете нам в течение следующих 48 часов.
Преобразите ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и приносит результаты. В PSS-Studio мы воплощаем в жизнь сайты, которые интегрируют изысканный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет бросаться в глаза в Интернете.
Почему стоит предпочесть нас?
– Эксклюзивный дизайн: Подкрепите идентичность вашего бренда.
– Гибкость отображения: Оптимальный просмотр на любом устройстве.
– Оптимизация для поисковых систем: Увеличьте вашу видимость в результатах поиска.
– Непрерывная помощь: Мы постоянно доступны помочь вам на любой стадии.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие немедленно. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к непревзойденному сайту.
С сердечными пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и гарантирует успех. В PSS-Studio мы создаем сайты, которые сочетают в себе изысканный дизайн и надежную работу, гарантируя, что ваш бренд будет заметен в Интернете.
Почему стоит обратиться к нам?
– Индивидуальный дизайн: Усилите индивидуальность вашего бренда.
– Универсальное представление: Идеальное отображение на любом устройстве.
– Улучшение позиций в поисковых системах: Укрепите вашу позицию в результатах поиска.
– Круглосуточная поддержка: Мы всегда на связи помочь вам на любом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который вызывает интерес, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые объединяют элегантный дизайн и превосходную эффективность, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит довериться нам?
– Уникальный дизайн: Отразите характер вашего бренда.
– Адаптивность: Великолепное представление на любом устройстве.
– Оптимизация для поисковых систем: Заставьте заметить ваш бренд в результатах поиска.
– Постоянная поддержка: Мы постоянно доступны помочь вам на каждом этапе.
Специальное предложение: Используйте возможность бесплатной консультации и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Обновите ваше цифровое присутствие немедленно. Посетите нас на https://pss-studio.ru/, чтобы начать ваше путешествие к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который захватывает дух, но и гарантирует успех. В PSS-Studio мы проектируем сайты, которые гармонично соединяют элегантный дизайн и надежную работу, гарантируя, что ваш бренд будет привлекать внимание в Интернете.
Почему стоит предпочесть нас?
– Особенный дизайн: Усилите индивидуальность вашего бренда.
– Гибкость отображения: Великолепное представление на любом устройстве.
– SEO-оптимизация: Расширьте ваше присутствие в результатах поиска.
– Готовность помочь в любой момент: Мы всегда к вашим услугам помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и особую скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Трансформируйте ваше цифровое присутствие уже сегодня. Ознакомьтесь с нашим предложением на https://pss-studio.ru/, чтобы пройти путь к выдающемуся сайту.
С теплыми пожеланиями, PSS.
Представьте себе сайт, который притягивает взгляды, но и обеспечивает эффективность. В PSS-Studio мы проектируем сайты, которые интегрируют непревзойденный стиль и высокую производительность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Индивидуальный дизайн: Отразите характер вашего бренда.
– Мобильная адаптация: Превосходное отображение на любом устройстве.
– Оптимизация под поисковики: Увеличьте вашу видимость в результатах поиска.
– Круглосуточная поддержка: Мы всегда готовы помочь вам на каждом этапе.
Специальное предложение: Воспользуйтесь бесплатной консультацией и эксклюзивную скидку на наши услуги по разработке сайтов, если ответите в течение следующих 48 часов.
Перевоплотите ваше цифровое присутствие сегодня. Зайдите на наш сайт на https://pss-studio.ru/, чтобы начать путь к непревзойденному сайту.
С наилучшими пожеланиями, PSS.
Представьте себе сайт, который сразу же запоминается, но и способствует вашему росту. В PSS-Studio мы проектируем сайты, которые объединяют элегантный дизайн и безупречную функциональность, гарантируя, что ваш бренд будет оставаться незабываемым в Интернете.
Почему стоит выбрать нас?
– Особенный дизайн: Подчеркните уникальность вашего бренда.
– Универсальное представление: Великолепное представление на любом устройстве.
– SEO-оптимизация: Повысьте ваш рейтинг в результатах поиска.
– Постоянная поддержка: Мы всегда рады помочь вам на всех этапах.
Специальное предложение: Запишитесь на бесплатную консультацию и уникальную скидку на наши услуги по разработке сайтов, если дадите обратную связь в течение следующих 48 часов.
Измените ваше цифровое присутствие сегодня. Посетите нас на https://pss-studio.ru/, чтобы отправиться в путешествие к замечательному сайту.
С теплыми пожеланиями, PSS.
Межрегиональный педагогический форум «Человек в цифровом мире» – это возможность обсудить актуальные вопросы цифровой трансформации образования и познакомиться с новыми решениями, столь актуальными для динамично меняющегося мира. Испытание пандемией обнажило главные проблемы цифровизации: неравенство образовательных систем и ключевую роль педагога в организации дистанционного обучения https://ito-kaliningrad.ru/.
Рассчитайте стоимость и время доставки вашего груза https://box-send.ru/.
Сэкономьте на покупке товара до 50% и получите возможность купить то, что нельзя сейчас купить в России https://box-send.ru/.
Криминалистика — прикладная юридическая наука, исследующая закономерности приготовления, совершения и раскрытия преступлений, возникновения и существования его следов, собирания, исследования, оценки и использования доказательств https://criminalistics-ed.ru/.
Здравствуйте, расскажите, пожалуйста, почему такая низкая цена на эти наушники https://applewatches.ru/?
Криминалистика — прикладная юридическая наука, исследующая закономерности приготовления, совершения и раскрытия преступлений, возникновения и существования его следов, собирания, исследования, оценки и использования доказательств, а также разрабатывающая систему основанных на познании этих закономерностей специальных приёмов, методов и средств применяемых в ходе предварительного расследования для предупреждения, раскрытия и расследования преступлений, а также при рассмотрении уголовных дел в судах https://criminalistics-ed.ru/.
https://positiv-servis.ru/
Рассчитайте стоимость и время доставки вашего груза https://box-send.ru/.
Купить мебель по доступной цене в Екатеринбурге, ХМАО, ЯНАО. Мебель из Китая, Малайзии, Белоруссии, Италии и России в магазине мебели КЛАССИКА https://www.classika-home.ru/.
Готовы погрузиться в мир магии?? Если ваш ребёнок грезит о волшебной палочке и каждый год ждёт письмо из Хогвартса, встреча с юным волшебником придётся ему по душе! Дети абсолютно всех возрастов любят Гарри. Отличным дополнение станет детективно-азотное или научное шоу https://yana-prazdnik.ru/!
Следите за нами в социальных сетях https://mega-connect.ru/.
ОПЕРАТИВНО Обработаем ваш заказ в течение 30 минут и оперативно доставим по нужному адресу https://shekswood.ru/.
Возьмем на обслуживание (купим, восстановим) УЖД с гарантированным грузооборотом https://rust-loco.ru/.
Здравствуйте! Огромное спасибо за ремонт, начало которого производил “чудо-мастер”. Работы по переделке и исправлению произведены быстро и очень грамотно. Вы настоящие профессионалы: с вами мы всегда понимали, что мы увидим по завершению работ. Если честно, этот ремонт в какой-то степени и воплощение желаний, чтобы нашей дочурке было уютно и комфортно! И конечный результат оказался таким, каким мы его хотели видеть. Благодарим за произведенный ремонт. Вы для нас – просто находка https://homeofdream.ru/!
ejbZRDNm
Волшебная Эльза поражает всех гостей праздника своей красотой и изяществом наряда https://yana-prazdnik.ru/.
Также важную роль играет зрение – штукатур должен уметь отличать цвета, даже на полутон и замечать мельчайшие дефекты поверхности https://statshtukatur.ru/.
Ресторан «Токио» сочетает в себе гармонию духа Японии и самобытную японскую культуру, так как можно с уверенностью сказать, что именно этот старейший ресторан более 25 лет назад познакомил Москву с истинной японской кухней https://ron-tokyo.ru/.
Сегодня ресторан «Токио» располагается в самом историческом центре Москвы, вблизи Арбата, в уютном особняке https://ron-tokyo.ru/.
Аудитория проекта — журналисты которые освещают проблемы науки и промышленности, организации и заводы, руководящий и рабочий состав предприятий, экономисты, аналитики, рекламщики, люди которых интересует наука и (или) промышленность, Все кому просто интересно, что то новое https://pjclub.ru/.
Требуется логотип для салона красоты в Москве!Название салона IMG Studio (зарегистрированный) https://ogologo.ru/.
Всё началось в конце 60-х годов в нью-йоркском Гарлеме, районе, который ассоциируется в нашем сознании с негритянской музыкой и джазом https://sibsalsa.ru/.
В лого должны быть графическое изображение женщины, желательно и мужчины,а также креативно расположенные буковки https://ogologo.ru/.
Определить сальсу одним словом довольно трудно: попробуйте сами в двух словах рассказать о музыке и танце https://sibsalsa.ru/.
Современное оборудование и опытные специалисты – наша гарантия качества. Каждая партия проходит проверку у начальника производства перед отправкой к клиенту https://shekswood.ru/.
ИНДИВИДУАЛЬНО Наши специалисты вникнут в Ваши потребности и подберут именно тот материал, который отвечает Вашим требованиям и нуждам https://shekswood.ru/.
Мы рады пригласить вас к сотрудничеству и готовы предложить вам разнообразные возможности для творческого подхода к осуществлению добрых дел https://milost-fond.ru/.
Оставьте свой e-mail, чтобы не пропустить Mega Connect 2022 и быть в курсе мепроприятий McKinsey https://mega-connect.ru/.
Квартирник Mega Connect 2021 Завершен https://mega-connect.ru/.
IV Региональный отборочный этап RoboCup Южного и Северо-Кавказского федеральных округов в рамках XVIII-ой Всероссийской научно-практической конференции “Перспективные системы и задачи управления” https://robocupdombay-otbor4.ru/.
«Промедиа, сетевые коммуникации» компания по разработке и созданию сайтов для малого бизнеса, промышленных, торговых, научно-производственных предприятий и предприятий сферы услуг Обнинска и Калужской области. Сделать сайт у нас – создать полноценный коммуникационный инструмент между вашим бизнесом и вашими клиентами в интернете https://promedia-site.ru/.
Дизайн в строительстве, архитектуре, городской среде и интерьере https://enidtp.ru/.
Школа, в которой мы учимся превращать нашу повседневность в искусство жизни https://perfectyear.ru/.
Поддерживая проект, вы вносите вклад в увеличение количества грантовых мест на курсы школы для того, чтобы финансовые ограничения не становились препятствием на пути личной трансформации для людей, готовых к изменениям https://perfectyear.ru/.
Получается, эти наушники 2010 года? Просто, компании beats и monster распались в 2010 году, и с 2012 года на наушниках beats нет ни слова о monster https://applewatches.ru/.
Более 500 таксопарков готовы выполнять ваш заказ https://huskytaxi.ru/.
У меня только-только закончился ремонт! Это было не так ужасно, как я думала, когда это все начиналось!! Мне попались на удивление ОТЛИЧНЫЕ строители!!!!!!!!! Делали ремонт “под ключ” в новостройке. Сделали СУПЕР!!! У мастера золотые руки! Если кому нужно, звоните ему. Сама знаю, как это, выискивать строителей в Москве. Могу скинуть фотки ремонта! ТАК ЧТО, ПИШИТЕ МНЕ, Я ВАМ ПОРЕКОМЕНДУЮ https://homeofdream.ru/!
О себе могу сказать, что я человек очень требовательный, даже придирчивый до занудности, но у мастера хватило терпения и такта реализовать все мои замечания и пожелания. Его работоспособность, когда он работал с 10.00 до 20.00, поразила меня и приятно порадовала сокращением сроков на ремонт. Большое спасибо мастеру https://homeofdream.ru/.
Дельтапланеризм это не только экстрим, это также возможность наслаждаться полетом, парить вместе с птицами, изучать тонкости погоды, и конечно же почувствовать какие облака на ощупь https://deltaextreme.ru/.
ASHLEY (Американская корпусная и мягкая мебель) https://www.classika-home.ru/.
Вместе вы погрузитесь в мир удивительных приключений и анимации. Идеально подходит для самых дружных и смелых поклонников мультфильма «Холодное сердце» https://yana-prazdnik.ru/.
Специалист должен быть аккуратным и иметь художественный вкус https://statshtukatur.ru/.
ПиДжиКлаб основан в 2008 году https://pjclub.ru/.
Цвета черный,оранжевый,белый,серый.Логотип общего значения, то есть будет использоваться на вывеске,визитках,меню и тд https://ogologo.ru/.
Общественный благотворительный фонд Милость оказывает помощь детям, трудным подросткам, инвалидам и пенсионерам. Приглашаем к сотрудничеству спонсоров и благотворителей. Обращайтесь к нам, если Вам необходима помощь https://milost-fond.ru/.
Мы верим, что участие в благотворительности не только наполняет радостью жизнь людей, которым оказана помощь, оно согревает сердца самих благотворителей, наполняет их жизнь смыслом https://milost-fond.ru/.
Правила поведения при проведении экскурсий https://rust-loco.ru/.
Наша компания предлагает широкий спектр запчастей к узкоколейной железнодорожной технике, а так же новый подвижной состав https://rust-loco.ru/.
Закрытие соревнований и награждение победителей: 7 апреля 2023 года https://robocupdombay-otbor4.ru/.
Перед тем, как «заказать» сайт чрезвычайно важно заложить базу, фундамент ресурса. При проектировании фундамента сайта нет необходимости уделять много внимания технической стороне функционирования будущего ресурса, визуальному оформлению и прочими вспомогательными вопросами. Тем не менее, на данном этапе важно согласовывать предполагаемые решения с веб-мастером https://promedia-site.ru/.
Онлайн-школа «Совершенный день» ставит перед собой цель помогать как можно большему количеству людей улучшать свою повседневность и обретать личную силу и уверенность https://perfectyear.ru/.
Избранные и последние поездки доступны в одно касание https://huskytaxi.ru/.
Первый сервис для заказа такси https://huskytaxi.ru/.
Дельтопланеризм – это невероятные возможности для преодоления сотен километров в парящем полете в горах и над равниной, используя лишь только то, что человек может унести с собой https://deltaextreme.ru/.
Криминалистика — прикладная юридическая наука, исследующая закономерности приготовления, совершения и раскрытия преступлений https://criminalistics-ed.ru/.
AP 91(Классическая, современная и мебель в стиле арт-деко из Китая и Азии) https://www.classika-home.ru/.
Заказывала наушники monster beats wireless неделю назад, хотела именно беспроодные https://applewatches.ru/.
Наши специалисты вникнут в Ваши потребности и подберут именно тот материал, который отвечает Вашим требованиям и нуждам https://shekswood.ru/.
Обработаем ваш заказ в течение 30 минут и оперативно доставим по нужному адресу https://shekswood.ru/.
Возьмем на обслуживание (купим, восстановим) УЖД с гарантированным грузооборотом https://rust-loco.ru/.
Наша компания предлагает все необходимое оборудование для торфодобычи https://rust-loco.ru/.
Сделать сайт у нас – создать полноценный коммуникационный инструмент между вашим бизнесом и вашими клиентами в интернете https://promedia-site.ru/.
Для владельцев или управляющих коммерческим проектом, сделать сайт для бизнеса – в подавляющем большинстве случаев означает создать ресурс, который поисковые системы будут предлагать аудитории ваших потенциальных клиентов https://promedia-site.ru/.
Более 500 таксопарков готовы выполнять ваш заказ https://huskytaxi.ru/.
Первый сервис для заказа такси https://huskytaxi.ru/.
Здравствуйте! Огромное спасибо за ремонт, начало которого производил “чудо-мастер”. Работы по переделке и исправлению произведены быстро и очень грамотно. Вы настоящие профессионалы: с вами мы всегда понимали, что мы увидим по завершению работ. Если честно, этот ремонт в какой-то степени и воплощение желаний, чтобы нашей дочурке было уютно и комфортно! И конечный результат оказался таким, каким мы его хотели видеть. Благодарим за произведенный ремонт. Вы для нас – просто находка https://homeofdream.ru/!
Дельтапланерный спорт – лучший выбор для тех, кто на пути к совершенству предпочитает красоту и изящность https://deltaextreme.ru/.
Дельтапланерный центр Delta Extreme, образованный на базе дельтаклуба Дельтаплан Московского Авиционного Института, проводит обучение полетам по расширенной программе подготовки спортсменов-дельтапланеристов https://deltaextreme.ru/.
Выполнение инжиниринговых услуг по оформлению разрешительной документации https://techair-as.ru/.
Начинали с небольших объемов строительства офисных помещений, реконструкции и возведения жилья https://vesta2.ru/.
Хотя сами латиноамериканцы это попытались сделать уже в самом названии: дело в том, что «сальса» [salsa] по-испански — это «соус», вещь, олицетворяющая для латинов всяческую смесь https://sibsalsa.ru/.
Издание зарегистрировано как средство массовой информации Федеральной службой по надзору в сфере связи и массовых коммуникаций (свидетельство о регистрации:Эл №ФС77-33749 от 24 октября 2008 г.) https://enidtp.ru/.
Поддерживая проект, вы вносите вклад в увеличение количества грантовых мест на курсы школы для того, чтобы финансовые ограничения не становились препятствием на пути личной трансформации для людей, готовых к изменениям https://perfectyear.ru/.
На нашем сайте предоставлены учебные материалы для студентов, по криминалистике https://criminalistics-ed.ru/.
Криминалистика — прикладная юридическая наука, исследующая закономерности приготовления преступлений https://criminalistics-ed.ru/.
Самые популярные герои, стильные костюмы, анимация с развивающими элементами, фокусник, научное шоу, бумажное шоу, пузыри, слаймы, аквагрим – все для восторга Вашего именинника и гостей https://yana-prazdnik.ru/.
Franchesko Mobili (Классическая мягкая мебель)https://classika-home.ru/.
Аутентичность и высочайшее качество неизменно являются фирменным отличием ресторана «Токио» https://ron-tokyo.ru/.
Всё началось в конце 60-х годов в нью-йоркском Гарлеме, районе, который ассоциируется в нашем сознании с негритянской музыкой и джазом https://sibsalsa.ru/.
Цены на проживание на Спортивно-оздоровительной базе «Домбай» https://robocupdombay-otbor4.ru/.
Издание включено в систему российского индекса научного цитирования (РИНЦ) и регулярно предоставляет полные тексты опубликованных статей по установленной форме в научную электронную библиотеку https://enidtp.ru/.
Определить сальсу одним словом довольно трудно: попробуйте сами в двух словах рассказать о музыке и танце https://sibsalsa.ru/.
Портативная акустика JBL on beat Black (Черный) https://applewatches.ru/.
Для того чтобы принять участие, заполните заявку, предоставленную ниже, и отправьте на почтуhttps://robocupdombay-otbor4.ru/.
Фотография лэндинга принадлежит фотостоку Unsplash https://robocupdombay-otbor4.ru/.
Онлайн-школа «Совершенный день» ставит перед собой цель помогать как можно большему количеству людей улучшать свою повседневность и обретать личную силу и уверенность https://perfectyear.ru/.
О себе могу сказать, что я человек очень требовательный, даже придирчивый до занудности, но у мастера хватило терпения и такта реализовать все мои замечания и пожелания. Его работоспособность, когда он работал с 10.00 до 20.00, поразила меня и приятно порадовала сокращением сроков на ремонт. Большое спасибо мастеру https://homeofdream.ru/.
У меня только-только закончился ремонт! Это было не так ужасно, как я думала, когда это все начиналось!! Мне попались на удивление ОТЛИЧНЫЕ строители!!!!!!!!! Делали ремонт “под ключ” в новостройке. Сделали СУПЕР!!! У мастера золотые руки! Если кому нужно, звоните ему https://homeofdream.ru/.
Штукатурные работы представляют — собой процесс нанесения на поверхность стены специального раствора, позволяющего скрыть неровности и загрунтовать поверхность перед чистовой отделкой https://statshtukatur.ru/.
В 1992 году в гостинице «Россия», в самом центре Москвы открылся этот оазис японской эстетики, который сразу же по достоинству оценили как москвичи, так и гости столицы https://ron-tokyo.ru/.
ASHLEY (Американская корпусная и мягкая мебель) https://classika-home.ru/.
Компания “PHOTOBOOK”, производитель выпускных фотоальбомов, в связи с активным развитием бизнеса проводит конкурсный отбор ДИЗАЙНЕРОВ-ВЕРСТАЛЬЩИКОВ для изготовления дизайна фотоальбомов https://ogologo.ru/.
С 2011г. решением президиума ВАК Минобрнауки РФ журнал включен в Перечень ведущих рецензируемых научных журналов и изданий, в которых должны быть опубликованы основные научные результаты диссертаций на соискание ученой степени доктора и кандидата наук https://enidtp.ru/.
В.В.Соколов — первый проректор Московского государственного университета информационных технологий, радиотехники и электроники» (МИРЭА, МГУПИ), доктор физико-математических, наук, профессор https://enidtp.ru/.
Порадуйте себя и окружающих ослепительно красивой улыбкой! Воспользуйтесь акцией Кабинетное + Домашнее отбеливание https://dr-dent63.ru/!
Если вам нужна помощь в написании работы, то рекомендуем обратиться к профессионалам https://criminalistics-ed.ru/.
Чехол Borofone Crocodile Black Кожа для Apple iPad 2/new iPad 3 https://applewatches.ru/.
Cтильные костюмы, анимация с развивающими элементами, фокусник, научное шоу, бумажное шоу, пузыри, слаймы, аквагрим – все для восторга Вашего именинника и гостей https://yana-prazdnik.ru/.
Аниматоры Томск. Создаем счастливые эмоции детства с 2014 года https://yana-prazdnik.ru/.
Четырнадцать лет назад, создаваясь как небольшая частная строительная компания ЗАО «ВЕСТА-II» сделало ставку на собственные возможности и надежность партнерских взаимоотношений https://vesta2.ru/.
В Нижневартовске началась подготовка к ежегодному фестивалю искусств, труда и спорта «Самотлорские ночи», который пройдет с 15 по 17 июня 2018 года https://ugra-tourism.ru/.
Сегодня ресторан «Токио» располагается в самом историческом центре Москвы, вблизи Арбата, в уютном особняке https://ron-tokyo.ru/.
«Токио» по-прежнему несет почетное звание ресторана-пионера японской кухни в Москве, угощая своих, так полюбивших его, гостей настоящими японскими блюдами, приготовленными по старинным классическим рецептам https://ron-tokyo.ru/.
Автозимник в Северном районе НСО до озера Тенис с деревни Алёшинка готов для проезда легковых автомашин, первые машины вчера пошли https://fishing55.ru/.
Квартиры премиум-класса с отделкой на 2-й Звенигородской улице рядом с метро “Улица 1905 года”. На территории площадью 4,5 гектара расположено 8 новых жилых домов, 7 исторических зданий с инфраструктурой. Парковые зоны занимают более трети территории квартала https://lucky-savills.ru/.
Казалось бы, всё просто — резинки держат штангу, если подергать — держат плотно, значит стучать и брякать нечему https://garage44.ru/.
Оставьте свой e-mail, чтобы не пропустить Mega Connect 2022 и быть в курсе мепроприятий McKinsey https://mega-connect.ru/.
Наши партнеры https://ugra-tourism.ru/.
Технологии художественной обработки материалов https://enidtp.ru/.
Получить выполненную работу или консультацию специалиста по вашему учебному проекту https://criminalistics-ed.ru/.
Стойки стабилизатора, иначе называемые штангами https://garage44.ru/.
Сетевой переходник для евророзетки с английской или американской https://applewatches.ru/.
BANG & OLUFSEN BeoPlay A3 Black (черный) https://applewatches.ru/.
Что такое телевизионная антенна, наверное, не знают только малыши, что делают свои первые шаги по земле https://kirovsat.ru/.
Если есть необходимость в том, чтобы дверь в течение долгого времени была открыта, то можно выбрать длительную разблокировку https://adamsrite.ru/.
Группа Компаний ФИННЛАК, являясь официальным дилером концерна Tikkurila Oyj, предлагает строительно-бытовые и промышленные лакокрасочные материалы торговой марки Тиккурила оптом. Вся реализуемая продукция изготовлена с учетом климатических особенностей России, что обеспечивает длительные сроки эксплуатации на протяжении 15 – 20 лет https://finnlak.ru/.
Но при том вам нет необходимости думать об ангаре для воздушного судна, его техническом обслуживании https://blogstreetdog.ru/.
Добавлена новая опция чит-коды https://for-minecraft.ru/.
На сайте есть много необычных решений и хитростей от наших профи https://skbbank-kredit.ru/.
ПиДжиКлаб основан в 2008 году https://pjclub.ru/.
Мы верим, что участие в благотворительности не только наполняет радостью жизнь людей, которым оказана помощь, оно согревает сердца самих благотворителей, наполняет их жизнь смыслом https://milost-fond.ru/.
Внимание всех любителей игры FIFA 09 нашему сайту нужен организатор турнира English Primer League (season 2) https://fifa-pc.ru/.
За четырнадцать лет созидательного труда в строительном бизнесе города Москвы при участии нашей компании возведено свыше 20 объектов жилого и нежилого назначения https://vesta2.ru/.
Всемирно известная награда Comedy Wildlife Photography Awards. Здесь жюри выбирает самые смешные фотографии животных со всего мира, которые авторы снимков https://smotrimfoto.ru/.
Нужен логотип для фирмы, которая продаёт и укладывает напольные покрытия(линолеум, ковролин, ламинат) https://ogologo.ru/.
https://akpp-moscow.ru/
Высокий уровень квалификации персонала и мощный научный потенциал https://highmet.ru/
Экопоселение Радость на территории прилегающей к озерам Ежозеро и Надречозеро https://eco-joy.ru/
Пригласите резидентов Comedy Club Saint-Petersburg к себе на праздник! Наши артисты с удовольствием выступят на Вашем мероприятии с юмористическими номерами, сделав это событие запоминающимся https://eventcomedy.ru/!
Для достижения этой цели вам нужно потратить всего 10 минут на чтение этой страницы https://brositkuritlegko.ru/.
Дверь, оборудованная защелкой такого типа, оснащена снаружи и изнутри неподвижной ручкой, никак не связанной с замком и всегда открывается ключом https://adamsrite.ru/.
Добавлен новый тип мира – большие биомы https://for-minecraft.ru/.
Центр исследований в области образовательной политики «Эврика» проводит онлайн-лагерь для детей и молодежи, изучающих русский язык в странах СНГ и Евросоюза https://centereureka.ru/.
Кодировка дисульфирамом — самый радикальный способ выработать стойкое и длительное отвращение к алкоголю https://otkapka.ru/.
Втулки стабилизатора — деталь копеечная и меняется легко, однако часто им не уделяется должного внимания https://garage44.ru/.
Добавлена новая опция бонусный сундук https://for-minecraft.ru/.
У мастеров компании «Штукатур Строй» есть все, чтобы штукатурные работы прошли быстро и надежно, включая многолетний опыт и профессиональные инструменты. Также специалисты знают, где искать недорогие и качественные стройматериалы, при необходимости они даже купят их за вас https://statshtukatur.ru/.
Серия фотографий, которая запечатлела выражение радости на мордах собак, когда им бросают угощение. Сегодня мы с помощью немецкого фотографа Кристиана https://smotrimfoto.ru/.
«Клуб промышленной журналистики» https://pjclub.ru/.
Каждое воскресение в 17:40 (по мск) на телеканале «Россия-Культура» выходит телешоу-викторина учителей «Передача знаний» https://sch11-33.ru/.
Созданная специально для женщин большого города, косметика NIO CITY оберегает твою кожу от городских стрессов, предотвращая их негативные последствия и возвращая коже свежий сияющий вид https://niocitymsk.ru/.
Мы рады пригласить вас к сотрудничеству и готовы предложить вам разнообразные возможности для творческого подхода к осуществлению добрых дел https://milost-fond.ru/.
Квартирник Mega Connect 2021 https://mega-connect.ru/.
Главная отличительная особенность лакокрасочных материалов торговой марки Тиккурила заключается в выпуске экологически чистых материалов, в соответствии с Международной программой по обеспечению технической безопасности, охране труда и окружающей среды. Кроме этого, ЛКМ изготовлены в полном соответствии мировым стандартам в области разработки и производства. Высокое качество подтверждено рядом европейских и российских сертификатов https://finnlak.ru/.
Этот матч определить многое в этой группе, команды находятся очень близко на расстоянии 2 очков. Команда России на данный момент идёт второй, а Финляндия третьей https://fifa-pc.ru/.
Я пытался устроиться на хорошую работу, но оказалось, что туда не берут курящих людей https://brositkuritlegko.ru/.
Электромеханические защелки для дверей незаменимы там, где наблюдается очень интенсивный поток входящих и выходящих людей. Для аварийных выходов такие устройства также идеально подходят https://adamsrite.ru/.
Комплексные штукатурные работы любой сложности https://statshtukatur.ru/.
Проверенные поставщики оборудования и материалов https://techair-as.ru/.
1 апреля открывается запись детей в первый класс. Напомним, прием детей в первый класс сейчас проходит в два этапа https://sch11-33.ru/.
Аудитория проекта — журналисты которые освещают проблемы науки и промышленности, организации и заводы, руководящий и рабочий состав предприятий, экономисты, аналитики, рекламщики, люди которых интересует наука и (или) промышленность, Все кому просто интересно, что то новое https://pjclub.ru/.
Требуется логотип для салона красоты в Москве!Название салона IMG Studio (зарегистрированный) https://ogologo.ru/.
Мы счастливы приветствовать Вас на сайте Санкт-Петербургского общественного благотворительного фонда «МИЛОСТЬ» https://milost-fond.ru/.
Здравствуйте, сегодня рыбачили в Барабаново на спиннинг с лодки. Народу много, насчитали около 40 лодок https://fishing55.ru/.
Следите за нами в социальных сетях: https://mega-connect.ru/.
Наши артисты имеют опыт ведения мероприятий любого уровня и масштаба https://eventcomedy.ru/.
При установке двух имплантов, на второй имплантат предоставляется 20% скидка! Акция действует до конца лета https://dr-dent63.ru/.
Разрабатываем идей контента и создания увлекательных текстов для оптимизации под поисковые системы https://digitalrush.ru/.
Во время бронирования вы считаетесь хозяином своего авиатранспорта https://blogstreetdog.ru/.
При подаче напряжения фиксатор электрозащелки разблокируется и дверь может быть открыта. Когда же дверь захлопывается, ригель защелкивается, и дверь оказывается надежно заперта https://adamsrite.ru/.
Арктическая зона имеет стратегическое значение для рыбохозяйственного комплекса России https://ryba29.ru/.
Квартал Лаки состоит из двух частей: верхнего и нижнего города, где удачно переплелись жилые и инфраструктурные объекты https://lucky-savills.ru/.
Необходимым условием развития Арктики является сохранение традиционных видов хозяйственной деятельности, рациональное использование водных биологических ресурсов, увеличение объемов и видов научных исследований, повышение их эффективности https://ryba29.ru/.
Поскольку стабилизатор включается в работу когда правое и левое колеса поджаты по-разному, при таком тесте стойки стаба застучат при езде под углом, а при проезде прямо будут молчать или вести себя явно тише https://garage44.ru/.
Boho coffee у Гиперболы, ТРЦ Гринвич, 8 марта, 46, 0 этаж, напротив Гиперболы https://bohoekb.ru/.
Сайт – не картина, внешним видом которой любуются прохожие. Это в первую очередь информационное поле, каждый сантиметр которого мы заполняем и обновляем с толком https://s-day.ru/!
Принципы ответственного управления рыбной отраслью крайне важно использовать при реализации всех крупных инфраструктурных инвестпроектов в Арктической зоне https://ryba29.ru/.
Добавлены новые структуры : храм в пустыне и в джунглях https://for-minecraft.ru/.
Мы работаем на Итальянском кофе Danesi. Неповторимый заветный купаж, в котором сочетаются зерна арабики высшего качества со сложным ароматомhttps://bohoekb.ru/.
Квалифицированные инженеры-проектировщики и монтажники https://techair-as.ru/.
Установка и обслуживание газовых котлов, газификация, газовое оборудование, отопление и водопровод в Ростове-на-Дону https://strgaz.ru/.
Выполнение инжиниринговых услуг по оформлению разрешительной документации https://techair-as.ru/.
В День России Владимир Путин поздравил югорчан с 900-летием первого упоминания Югры в русском летописании, отметив особую роль автономного округа в развитии страны https://ugra-tourism.ru/.
Подключение спутникового ТВ https://kirovsat.ru/.
ЗАО «ВЕСТА-II», в соответствии разрешенными видами деятельности на основании выданных лицензий обеспечивают полный цикл работ по сопровождению проекта на всех этапах реализации от разработки и утверждения исходно-разрешительной документации до ввода объекта в эксплуатацию https://vesta2.ru/.
В глазах клиентов у вас нет конкурентов. Мощные составляющие фирменного стиля переводят все внимание исключительно на вас https://s-day.ru/.
Вчера в Индии начался фестиваль огней Дивали (Diwali), который приходится на начало месяца Картик (октябрь—ноябрь). Дивали на санскрите означает «огненная” https://smotrimfoto.ru/.
Этот район является одним из главных рыбодобывающих макрорегионов – девять арктических субъектов обеспечивают около 17% улова по стране https://ryba29.ru/.
Начну с терминов, чтобы не было путаницы. Если, к примеру, находясь за обеденным столом, разговариваешь с белочкой, а на столе сидит кот, ну или…https://fishing55.ru/
Выведение из запоя и снятие похмельного синдрома в день обращения в клинику https://otkapka.ru.
Жизнь в мегаполисе — это не только большие возможности, но и большие стрессы https://niocitymsk.ru/.
Верхний город – это восемь жилых домов, квартиры в которых предлагаются с отделкой https://lucky-savills.ru/.
Ассортимент продукции концерна Тиккурила включает лакокрасочные материалы для широкого круга потребителей. Многообразная палитра красок, большой выбор лаков, грунтовок, текстурных покрытий, антисептиков, шпатлевки и других продуктов – все это дает возможность выбрать полный спектр материалов, необходимых для декоративного оформления строительных конструкций, зданий, помещений и их защиты от коррозии или других дефектов Ассортимент продукции концерна Тиккурила включает лакокрасочные материалы для широкого круга потребителей. Многообразная палитра красок, большой выбор лаков, грунтовок, текстурных покрытий, антисептиков, шпатлевки и других продуктов – все это дает возможность выбрать полный спектр материалов, необходимых для декоративного оформления строительных конструкций, зданий, помещений и их защиты от коррозии или других дефектов https://finnlak.ru/.
Сегодня на стадионе Динамо им. В.В. Лобановского пройдёт отборочный матч на Чемпионат Мира 2010 https://fifa-pc.ru/.
Наши резиденты являются участниками популярных телепроектов: Comedy Club, Comedy Баттл, Не Спать, Убойная Лига, Смех Без Правил и многие другие https://eventcomedy.ru/!
Пусть еще я очень мал,Но в душе я генерал!Генералом буду важным,Сильным, храбрым и отважным!Буду я всех защищать,Долг свой смело выполнять!А пока что долг один —Поздравлять мне всех мужчин.С гордостью скажу вам я:С 23 Февраля https://detskiisad53.ru/!
Профессиональная гигиена полости рта + профессиональное кабинетное отбеливание https://dr-dent63.ru/.
Мы специализируемся на оказании помощи компаниям в повышении их видимости в Интернете путем оптимизации контента под ключевые слова, создания обратных ссылок с других сайтов https://digitalrush.ru/.
У меня появился постоянный кашель, стали
донимать головные боли и частые простуды https://brositkuritlegko.ru/.
Союз является некоммерческой организацией, созданной в целях саморегулирования, основанной на членстве, объединяющей субъектов предпринимательской деятельности, осуществляющих деятельность в области туристического бизнеса и сопутствующих направлениях деятельности https://ugra-tourism.ru/.
На сегодняшний день, наша компания не самая крупная по московским меркам, полностью обеспечивает свои объекты финансированием, материалами, высококвалифицированным персоналом и имеет репутацию крепкой и надежной компании https://vesta2.ru/.
Мир становится быстрее и безумнее, и по всему миру можно встретить людей, заснувших в самых разных, порой абсолютно неожиданных, местах https://smotrimfoto.ru/.
Если вы путешествуете частным авиасудном редко, то бронировать его рентабельнее, чем обслуживать https://blogstreetdog.ru/.
Сегодня государство уделяет приоритетное внимание развитию рыбохозяйственного комплекса https://ryba29.ru/.
Обсуждайте и задавайте ваши вопросы, мы всегда поможем вам https://skbbank-kredit.ru/!
Для многих проблема алкоголизма стоит очень остро, но от судьбоносного решения обратиться к специалисту их удерживает опасение огласки или нежелание https://otkapka.ru.
По статистике, кожа горожан более склонна к воспалениям, закупориванию пор, акне, пигментации, тусклому цвету и преждевременному старению https://niocitymsk.ru/.
Целью Академии является содействие членам в осуществлении деятельности в области жилищно-коммунального хозяйства, бытового обслуживания и экологии, объединение усилий в создании мультипликативного эффекта выраженного в развитии и модернизации жилищного фонда, эффективном использовании коммунальных ресурсов, создании благоприятного инвестиционного климата и совершенствования институциональной среды ЖКХ. https://www.acgkh.ru/
В нижнем городе расположено все самое важное для качественной жизни: фермерские магазины, театр, детский сад, а также художественные студии, школы для изучения иностранных языков и подогреваемый бассейн на крыше https://lucky-savills.ru/.
Полный технологический цикл от сырья до готовой продукции https://highmet.ru/
Диагностика стоек стабилизатора проста — проезжаем по лежачему полицейскому или рельсам сначала прямо а затем под углом https://garage44.ru/.
Наши артисты проведут мероприятие любого уровня: свадьба, корпоративный вечер, презентация, день рождения или празднование Нового года https://eventcomedy.ru/!
Индивидуальный подход в решении технических задач https://techair-as.ru/.
Всероссийский праздник День семьи, любви и верности тесно связан с историей и жизнеописанием святых благоверных Петра и Февронии. Эта супружеская чета жила в городе Муроме Владимирской области в XII-XIII веках https://detskiisad53.ru/.
Специальные предложения Стоматологической клиники “Доктор Дент”:
Скидка 20% на второй имплантат https://dr-dent63.ru/!
Мы помогаем нашим клиентам увеличить посещаемость сайта, рейтинг и видимость в результатах поиска https://digitalrush.ru/.
В ноябре будет проходить бесплатный онлайн-лагерь для детей и взрослых, изучающих русский язык https://centereureka.ru/.
Газовые котлы и приборы, отопление и газификация в Ростове https://strgaz.ru/.
Boho coffee у Стокманн, ТРЦ Гринвич, 8 марта, 46, 1 этаж, рядом с бывшим Стокманн https://bohoekb.ru/.
Строительство или капитальный ремонт сайтов – наша основная специализация. Ваше интернет-представительство должно впечатлять и продавать https://s-day.ru/.
Калуга с размахом отмечала 650-летие, и по такому прекрасному поводу над Яченским водохранилищем аккурат напротив музея космонавтики были устроен Кубок https://smotrimfoto.ru/.
Уважаемые родители и учащиеся! По настоятельной рекомендации Роспотребнадзора классы ,в которых хотя бы один ученик имеет подтвержденный Ковид, выводятся на 7 дней, организация обучения происходит с использованием дистанционных образовательных технологий https://sch11-33.ru/.
Мы собрали самые достойные решения и с радостью поделимся с Вами https://skbbank-kredit.ru/.
Высокий темп жизни и неблагоприятная экология снижают защитные функции организма https://niocitymsk.ru/.
Спутниковое ТВ в Кирове и Кировской области https://kirovsat.ru/.
Индивидуальный подход к каждому клиенту https://highmet.ru/
Место, где продуманы, учтены и вручную сконструированы тончайшие нюансы, из которых складываются комфорт и счастье https://lucky-savills.ru/.
В случае победы команды Гуса Хиддинка, его команда отрывается от их ближайший преследователей команды Финляндии на 5 очков. Если фортуна улыбнется Финляндии, то она выйдет на второе место, обогнав сборную России https://fifa-pc.ru/.
Исправлено огромное кол-во багов и ошибок https://for-minecraft.ru/.
Добро пожаловать на сайт Омских рыбаков – крупнейшее интернет-сообщество рыбаков в Сибири https://fishing55.ru/.
В целях активизации работы по профилактике детского дорожно-транспортного травматизма, обеспечения безопасности несовершеннолетних, а также адаптации детей к транспортной среде в местах постоянного жительства, в МБДОУ “Центр развития ребенка – детский сад №53” в период с 18 мая по 18 июня 2022 года https://detskiisad53.ru/.
Популяризация русского языка, российского образования и культуры через организацию, и проведение онлайн-лагеря для обучающихся русских школ за рубежом https://centereureka.ru/.
Группа Компаний ФИННЛАК, осуществляя свою деятельность на протяжении более 20 лет, сумела стать одним из самых успешных дистрибьюторов концерна Tikkurila Oyj в России Группа Компаний ФИННЛАК, осуществляя свою деятельность на протяжении более 20 лет, сумела стать одним из самых успешных дистрибьюторов концерна Tikkurila Oyj в России https://finnlak.ru/.
Но гораздо удобней использовать функцию электрического открывания электромеханической защелки https://adamsrite.ru/.
Сайт экопоселения РАДОСТЬ расположенного в Вытегорском районе Вологодской области https://eco-joy.ru/
В течение последующих 14 лет я не расставался с сигаретой ни на день https://brositkuritlegko.ru/.
В случае, когда во время рейса на авиасудне вам нужно общаться с партнерами по бизнесу, лучше отдать предпочтение данному виду бронирования https://blogstreetdog.ru/.
Разработка и реализация мероприятий, программ и проектов, включая социально-значимые, направленных на развитие и обеспечение благоприятных условий осуществления в сфере жилищно-коммунального хозяйства, бытового обслуживания и экологии https://www.acgkh.ru/
В День России Владимир Путин поздравил югорчан с 900-летием первого упоминания Югры в русском летописании, отметив особую роль автономного округа в развитии страны https://ugra-tourism.ru/.
Этот район является одним из главных рыбодобывающих макрорегионов – девять арктических субъектов обеспечивают около 17% улова по стране https://ryba29.ru/.
Кодировка дисульфирамом — самый радикальный способ выработать стойкое и длительное отвращение к алкоголю https://otkapka.ru/.
Втулки стабилизатора — деталь копеечная и меняется легко, однако часто им не уделяется должного внимания https://garage44.ru/.
Мы собрали самые достойные решения и с радостью поделимся с Вами https://skbbank-kredit.ru/.
Созданная специально для женщин большого города, косметика NIO CITY оберегает твою кожу от городских стрессов, предотвращая их негативные последствия и возвращая коже свежий сияющий вид https://niocitymsk.ru/.
В целях активизации работы по профилактике детского дорожно-транспортного травматизма, обеспечения безопасности несовершеннолетних, а также адаптации детей к транспортной среде в местах постоянного жительства, в МБДОУ “Центр развития ребенка – детский сад №53” в период с 18 мая по 18 июня 2022 года https://detskiisad53.ru/.
Boho coffee у Стокманн, ТРЦ Гринвич, 8 марта, 46, 1 этаж, рядом с бывшим Стокманн https://bohoekb.ru/.
Наши артисты имеют опыт ведения мероприятий любого уровня и масштаба https://eventcomedy.ru/.
Профессиональная гигиена полости рта + профессиональное кабинетное отбеливание https://dr-dent63.ru/.
Сайт – не картина, внешним видом которой любуются прохожие. Это в первую очередь информационное поле, каждый сантиметр которого мы заполняем и обновляем с толком https://s-day.ru/!
Проверенные поставщики оборудования и материалов https://techair-as.ru/.
Арктическая зона имеет стратегическое значение для рыбохозяйственного комплекса России https://ryba29.ru/.
Но гораздо удобней использовать функцию электрического открывания электромеханической защелки https://adamsrite.ru/.
Для многих проблема алкоголизма стоит очень остро, но от судьбоносного решения обратиться к специалисту их удерживает опасение огласки или нежелание https://otkapka.ru.
Начинали с небольших объемов строительства офисных помещений, реконструкции и возведения жилья https://vesta2.ru/.
Газовые котлы и приборы, отопление и газификация в Ростове https://strgaz.ru/.
Верхний город – это восемь жилых домов, квартиры в которых предлагаются с отделкой https://lucky-savills.ru/.
Всемирно известная награда Comedy Wildlife Photography Awards. Здесь жюри выбирает самые смешные фотографии животных со всего мира, которые авторы снимков https://smotrimfoto.ru/.
Исправлено огромное кол-во багов и ошибок https://for-minecraft.ru/.
1 апреля открывается запись детей в первый класс. Напомним, прием детей в первый класс сейчас проходит в два этапа https://sch11-33.ru/.
Высокий уровень квалификации персонала и мощный научный потенциал https://highmet.ru/
Этот матч определить многое в этой группе, команды находятся очень близко на расстоянии 2 очков. Команда России на данный момент идёт второй, а Финляндия третьей https://fifa-pc.ru/.
Мы работаем на Итальянском кофе Danesi. Неповторимый заветный купаж, в котором сочетаются зерна арабики высшего качества со сложным ароматомhttps://bohoekb.ru/.
Мы провели более 3000 мероприятий, обретя бесценный опыт создания и реализации уникальных концепций https://eventcomedy.ru/.
В Нижневартовске началась подготовка к ежегодному фестивалю искусств, труда и спорта «Самотлорские ночи», который пройдет с 15 по 17 июня 2018 года https://ugra-tourism.ru/.
При установке двух имплантов, на второй имплантат предоставляется 20% скидка! Акция действует до конца лета https://dr-dent63.ru/.
Строительство или капитальный ремонт сайтов – наша основная специализация. Ваше интернет-представительство должно впечатлять и продавать https://s-day.ru/.
Мы специализируемся на оказании помощи компаниям в повышении их видимости в Интернете путем оптимизации контента под ключевые слова, создания обратных ссылок с других сайтов https://digitalrush.ru/.
Сегодня государство уделяет приоритетное внимание развитию рыбохозяйственного комплекса https://ryba29.ru/.
При подаче напряжения фиксатор электрозащелки разблокируется и дверь может быть открыта. Когда же дверь захлопывается, ригель защелкивается, и дверь оказывается надежно заперта https://adamsrite.ru/.
Ассортимент продукции концерна Тиккурила включает лакокрасочные материалы для широкого круга потребителей. Многообразная палитра красок, большой выбор лаков, грунтовок, текстурных покрытий, антисептиков, шпатлевки и других продуктов – все это дает возможность выбрать полный спектр материалов, необходимых для декоративного оформления строительных конструкций, зданий, помещений и их защиты от коррозии или других дефектов Ассортимент продукции концерна Тиккурила включает лакокрасочные материалы для широкого круга потребителей. Многообразная палитра красок, большой выбор лаков, грунтовок, текстурных покрытий, антисептиков, шпатлевки и других продуктов – все это дает возможность выбрать полный спектр материалов, необходимых для декоративного оформления строительных конструкций, зданий, помещений и их защиты от коррозии или других дефектов https://finnlak.ru/.
Четырнадцать лет назад, создаваясь как небольшая частная строительная компания ЗАО «ВЕСТА-II» сделало ставку на собственные возможности и надежность партнерских взаимоотношений https://vesta2.ru/.
Выведение из запоя и снятие похмельного синдрома в день обращения в клинику https://otkapka.ru.
Серия фотографий, которая запечатлела выражение радости на мордах собак, когда им бросают угощение. Сегодня мы с помощью немецкого фотографа Кристиана https://smotrimfoto.ru/.
Место, где продуманы, учтены и вручную сконструированы тончайшие нюансы, из которых складываются комфорт и счастье https://lucky-savills.ru/.
На сайте есть много необычных решений и хитростей от наших профи https://skbbank-kredit.ru/.
Казалось бы, всё просто — резинки держат штангу, если подергать — держат плотно, значит стучать и брякать нечему https://garage44.ru/.
По статистике, кожа горожан более склонна к воспалениям, закупориванию пор, акне, пигментации, тусклому цвету и преждевременному старению https://niocitymsk.ru/.
Для достижения этой цели вам нужно потратить всего 10 минут на чтение этой страницы https://brositkuritlegko.ru/.
Полный технологический цикл от сырья до готовой продукции https://highmet.ru/
Добавлена новая опция бонусный сундук https://for-minecraft.ru/.
Внимание всех любителей игры FIFA 09 нашему сайту нужен организатор турнира English Primer League (season 2) https://fifa-pc.ru/.
Пусть еще я очень мал,Но в душе я генерал!Генералом буду важным,Сильным, храбрым и отважным!Буду я всех защищать,Долг свой смело выполнять!А пока что долг один —Поздравлять мне всех мужчин.С гордостью скажу вам я:С 23 Февраля https://detskiisad53.ru/!
Наши резиденты являются участниками популярных телепроектов: Comedy Club, Comedy Баттл, Не Спать, Убойная Лига, Смех Без Правил и многие другие https://eventcomedy.ru/!
Если вы путешествуете частным авиасудном редко, то бронировать его рентабельнее, чем обслуживать https://blogstreetdog.ru/.
Порадуйте себя и окружающих ослепительно красивой улыбкой! Воспользуйтесь акцией Кабинетное + Домашнее отбеливание https://dr-dent63.ru/!
Центр исследований в области образовательной политики «Эврика» проводит онлайн-лагерь для детей и молодежи, изучающих русский язык в странах СНГ и Евросоюза https://centereureka.ru/.
Мы помогаем нашим клиентам увеличить посещаемость сайта, рейтинг и видимость в результатах поиска https://digitalrush.ru/.
Boho coffee у Гиперболы, ТРЦ Гринвич, 8 марта, 46, 0 этаж, напротив Гиперболы https://bohoekb.ru/.
Электромеханические защелки для дверей незаменимы там, где наблюдается очень интенсивный поток входящих и выходящих людей. Для аварийных выходов такие устройства также идеально подходят https://adamsrite.ru/.
Разрешите представить: самый главный наш мальчик Гудквайтс Моушен ту Виктори, его преемник Тодес Блэк Даймонд, девочки Амулет Рею Лаки Миднайт, Тринити Джой Альциона, и наша подающая надежды молдодежь: Ригейн Найс Флауэр и Стенвейз Найтли Скай https://labradoriki.ru/.
Каждое воскресение в 17:40 (по мск) на телеканале «Россия-Культура» выходит телешоу-викторина учителей «Передача знаний» https://sch11-33.ru/.
ЗАО «Мегадента» – является одной из крупнейших стоматологических торгующих организаций в Российской Федерации. Мы организует марафоны, конгрессы и конференции, чтобы повышать качество стоматологического образования https://kongress-mgn.ru/.
Power Transmission® – это инновационный подход к работе, который позволяет решать все задачи в максимально короткие сроки https://akpp-moscow.ru/.
Компания «Шатер4you» предоставляет в аренду большой ассортимент оборудования для проведения любых видов выездных мероприятий https://shater4you.ru/.
Если вас заинтересовал наш подход к обучающим программам мы с удовольствием рассмотрим любой ваш запрос https://sabina-study.ru/.
Интернет – зоомагазин Котя Шоп специализируется на продаже кормов и аксессуаров для домашних животных. Вы всегда можете заказать как сухие корма для кошек и собак, так и влажные корма от различных производителей https://kotya-shop.ru/.
Стоимость доставки материалов в зависимости от места нахождения объекта https://maste-ru.ru/.
Если Вы хотите помочь ретриверу, оставшемуся без дома, обратите внимание на нашу КАРТОТЕКУ https://help-retriever.ru/.
Во время бронирования вы считаетесь хозяином своего авиатранспорта https://blogstreetdog.ru/.
Языковой курс «Сабина» создан для англоговорящих пользователей, позволяет познакомиться с основами узбекского языка в игровой форме https://sabina-study.ru/.
Многоуровневый потолок с фотопечатью https://positiv-servis.ru/.
Что такое телевизионная антенна, наверное, не знают только малыши, что делают свои первые шаги по земле https://kirovsat.ru/.
Мы отдаем предпочтение кормам премиум класса. Несмотря на более высокую стоимость по сравнению с кормами эконом класса, корма премиум класса имеют в составе ингредиенты высшего качества, витамины и минералы, за счет чего они легко усваиваются https://kotya-shop.ru/.
Стоматологическая ассоциация России (СтАР) – крупнейшая общественная организация в стране по принадлежности к одной врачебной специальности, объединяющая и координирующая действия по защите профессиональных и социальных прав специалистов стоматологического профиля в России https://kongress-mgn.ru/.
Здравствуйте, сегодня рыбачили в Барабаново на спиннинг с лодки. Народу много, насчитали около 40 лодок https://fishing55.ru/.
Любой груз застрахован
на 1 000 000 рублей https://box-send.ru/.
Двухуровневый потолок с фотопечатью https://positiv-servis.ru/.
Этот метод сервисного обслуживания мы переняли у американских партнёров, система CORE/Обмен у них существует уже не первый десяток лет, американцы не тратят время на ремонт – они покупают готовый продукт https://akpp-moscow.ru/.
12 мая компания Shater4you предоставила Московской Еврейской Общине в аренду шатры типа Пагода и банкетную мебель, стулья Селена и банкетные прямоугольные столы, для проведения мероприятия, посвященному дню Победы https://shater4you.ru/.
МЕХАНИЗИРОВАННАЯ ШТУКАТУРКА ФАСАДОВ https://maste-ru.ru/.
Программа создана на базе мультимедийной технологии Flash и призвана показать новые аспекты её применения https://sabina-study.ru/.
Белый глянцевый потолок https://positiv-servis.ru/.
КЛАДКА ГАЗОБЛОКА ПАЗОГРЕБНЯ КЕРПИЧА https://maste-ru.ru/.
Мы занимаемся лабрадорами черного и шоколадного окрасов. У наших собак есть свой ветеринарный врач, есть дрессировщик, знающий нюансы породы, хендлер. Мы работаем по программе “заводчик” с компанией Purina https://labradoriki.ru/.
Большой выбор сухих и влажных кормов учитывает все вкусовые предпочтения вашего любимца. Также в нашем магазине всегда найдутся специализированные корма для различных периодов жизни вашего питомца: корм для котят и щенков, корм для беременных кошек и собак, корм для пожилых и кастрированных животных https://kotya-shop.ru/.
Nobel Biocare – является мировым лидером в области инновационных ортопедических решений с применением дентальных имплантатов https://kongress-mgn.ru/.
Целью Академии является содействие членам в осуществлении деятельности в области жилищно-коммунального хозяйства, бытового обслуживания и экологии, объединение усилий в создании мультипликативного эффекта выраженного в развитии и модернизации жилищного фонда, эффективном использовании коммунальных ресурсов, создании благоприятного инвестиционного климата и совершенствования институциональной среды ЖКХ. https://www.acgkh.ru/
Пусть мы не сможем спасти всех, кого бы нам хотелось. Но мы спасем намного больше, чем те, кто даже не пытается https://help-retriever.ru/.
Привезем товары и бренды в любой город России. Дешевле и быстрее других компаний https://box-send.ru/.
Сэкономьте на покупке товара до 50% и получите возможность купить то, что нельзя сейчас купить в России https://box-send.ru/.
Выполнение инжиниринговых услуг по оформлению разрешительной документации https://techair-as.ru/.
Компания Power Transmission® (Пауэр Трансмишн) – инновационный подход к ремонту автоматических коробок передач https://akpp-moscow.ru/.
Подключение спутникового ТВ https://kirovsat.ru/.
Группа Компаний ФИННЛАК, осуществляя свою деятельность на протяжении более 20 лет, сумела стать одним из самых успешных дистрибьюторов концерна Tikkurila Oyj в России Группа Компаний ФИННЛАК, осуществляя свою деятельность на протяжении более 20 лет, сумела стать одним из самых успешных дистрибьюторов концерна Tikkurila Oyj в России https://finnlak.ru/.
Экопоселение Радость на территории прилегающей к озерам Ежозеро и Надречозеро https://eco-joy.ru/
У меня появился постоянный кашель, стали
донимать головные боли и частые простуды https://brositkuritlegko.ru/.
Но при том вам нет необходимости думать об ангаре для воздушного судна, его техническом обслуживании https://blogstreetdog.ru/.
Разработка и реализация мероприятий, программ и проектов, включая социально-значимые, направленных на развитие и обеспечение благоприятных условий осуществления в сфере жилищно-коммунального хозяйства, бытового обслуживания и экологии https://www.acgkh.ru/
Индивидуальный подход в решении технических задач https://techair-as.ru/.
Установка и обслуживание газовых котлов, газификация, газовое оборудование, отопление и водопровод в Ростове-на-Дону https://strgaz.ru/.
Уважаемые родители и учащиеся! По настоятельной рекомендации Роспотребнадзора классы ,в которых хотя бы один ученик имеет подтвержденный Ковид, выводятся на 7 дней, организация обучения происходит с использованием дистанционных образовательных технологий https://sch11-33.ru/.
Спутниковое ТВ в Кирове и Кировской области https://kirovsat.ru/.
Автозимник в Северном районе НСО до озера Тенис с деревни Алёшинка готов для проезда легковых автомашин, первые машины вчера пошли https://fishing55.ru/.
Группа Компаний ФИННЛАК, являясь официальным дилером концерна Tikkurila Oyj, предлагает строительно-бытовые и промышленные лакокрасочные материалы торговой марки Тиккурила оптом. Вся реализуемая продукция изготовлена с учетом климатических особенностей России, что обеспечивает длительные сроки эксплуатации на протяжении 15 – 20 лет https://finnlak.ru/.
Сайт экопоселения РАДОСТЬ расположенного в Вытегорском районе Вологодской области https://eco-joy.ru/
Я пытался устроиться на хорошую работу, но оказалось, что туда не берут курящих людей https://brositkuritlegko.ru/.
https://sabina-study.ru/
能告知一下paper title或者PMID号吗